- Update – My book Overcoming Tendonitis: A Systematic Approach to the Evidence-Based Treatment of Tendinopathy is on Amazon, and the digital edition in my store.
- Update 2 – Medial elbow (golfer’s elbow, climber’s elbow, etc) 8-12 week Video Rehab Program has been released!
Tendonitis is one of the most pesky injuries that can plague an athletes career, which can derail both practice and performance. This article seeks to explore the mechanisms of tendonitis and how to successfully implement a rehabilitation plan to overcome tendonitis backed by current scientific research and best practices in the clinic.
Table of Contents
- How Tendonitis develops
- Symptom severity
- Common misconceptions about tendinopathy rehabilitation
- General summary of studies on tendinopathy
- Do you have potential tendinopathy with chronic pain?
- Corrective measures — eccentric exercises and peripheral work
- Planning rehabilitative sessions — order of exercises and getting back to training
- Should I work through pain during rehabilitation?
- Should you continue your sport(s) while doing rehabilitation?
- Braces — do not treat the problem but may be effective in dealing with pain while continuing activity
- Supplements — things that may help
Latest updates:
- There are seven old posts with cases if you want to look for people who are sharing their cases or successes.
- May 2023 – This list got too long. Continuing to streamline this.
Disclaimer: Any information contained in this article should not be misconstrued as professional medical advice. Always consult your appropriate medical professional before using such information. Use of any information is at your own risk.
How Tendonitis develops
Tendonitis is an outdated term due to the fact that the condition is often described in the scientific literature as a “non-inflammatory proliferative disorder.” In other words, there is little to no inflammation present during the process of overuse of the tendon. The term used by most professionals now is Tendinopathy, which covers the broad spectrum of the degeneration of the tendon.
Here is a pictorial example of the process. Illustrations are ours from the book.
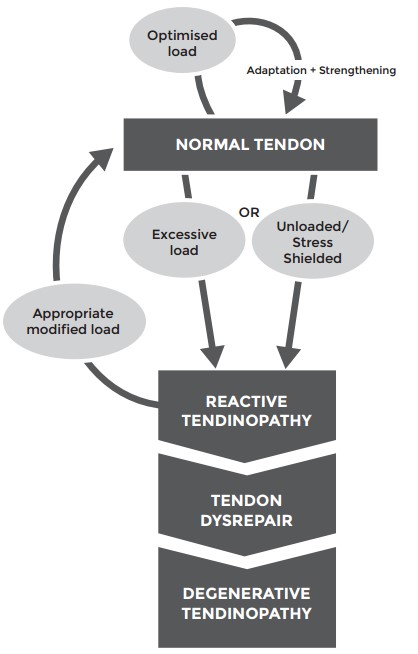
Original illustration from 2009 Cook and Purdam study. New image from Overcoming Tendonitis book.
Tendinopathy is an overuse injury. This condition arises when the volume of the workouts exceed your tendon’s ability to recover. Muscles and bones are more metabolically active than our connective tissue (tendons, ligaments, cartilage), so they often are able to adapt to the stressors of exercise placed on them faster. This can leave connective tissues and bones vulnerable to overuse since they cannot heal as fast. If excessive stress is placed on them, they start to react negatively to the stress. (I don’t use “have more blood flow” anymore because that is a misnomer).
Main takeaway: Load management via appropriately modified stress allows recovery from the tendinopathy.
Since this article was written (2010), there has been a lot more research into modeling the various ‘stages’ of tendinopathy and how they react to increased exercise and dysfunction. Here is the 2016 model from Cook with added information about the process while making it simpler.
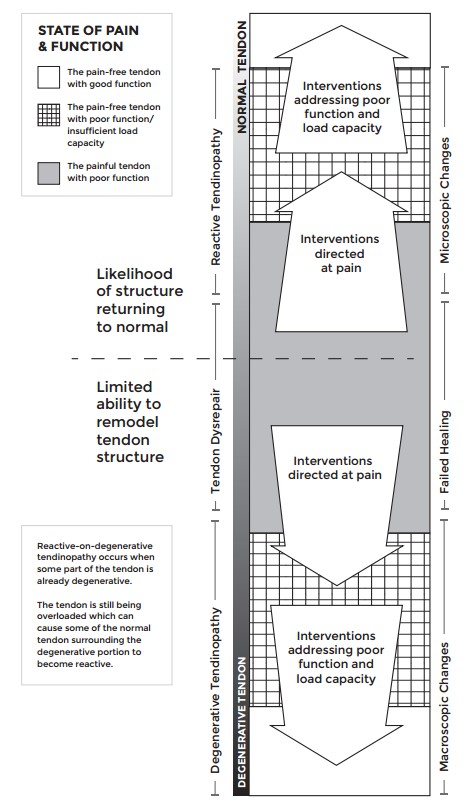
Original illustration in the Cook model study (Sept 2016). New image from Overcoming Tendonitis book.
Here are the stages explained:
- Tendinopathy starts out with stress being placed on the tendon from activity or workouts. If the stress overloads the ability of the tendon to adapt then reactive tendinopathy occurs.
- Reactive tendinopathy tends to exhibit signs and symptoms of tendonitis such as pain, soreness, achiness, and so on localized around the affected area. Symptoms generally go away with ceasing the aggravating exercises. If the loads on the tendon are appropriately modified, the tendon will be able to repair itself and move back into normal tendon stage. In this state, it is only possible to see degenerative changes under a microscope. This stage is generally referred to a non-inflammatory proliferative response to excessive loading: there may be a bit of inflammation present in the reactive tendinpathy stage but it is extremely limited and doesn’t cause dysfunction. In other words, there’s no such thing as “TENDON-ITIS“ despite the common use of the term.
- If excessive stress is continually placed on a tendon in reactive tendinopathy, it may start to progress into a tendon dysrepair state. Tendon disrepair occurs when excessive loads are applied to a tendon in the state of reactive tendinopathy. During this process, the normal repair mechanisms of the tendon in reactive tendinopathy are disrupted by continually applying overloading forces to the tendon, which results in a state of disrepair. An appropriate analogy for this would be continually pulling off scabs: it leads to the repair process being disrupted and more scabs continually being developed until there is obvious signs of scar tissue.
- Degenerative tendinopathy is the state of the tendon which has transitioned past a state of dysrepair. In this stage it is possible to see large scale disruptions in the tendon in imaging techniques such as MRI. There is typically dysfunctional or no inflammation present in the degenerative tendinopathy stage. There is limited reversibility of the degeneration. Large scale forces placed on a tendon in tendon disrepair, especially the degenerative tendinopathy stage, can lead to large scale tearing of the tendon resulting in grade II (partial) and grade III (full) tears.
Reactive on degenerative tendinopathy is a similar state where you may have an area of degenerative with reactive tendinopathy around it. This tendinopathy tends to “get better with rest” but then stops up to a point. The reason for this is that the reactive portion of the tendon resolves back to normal, but the degenerative portion cannot heal to normal.
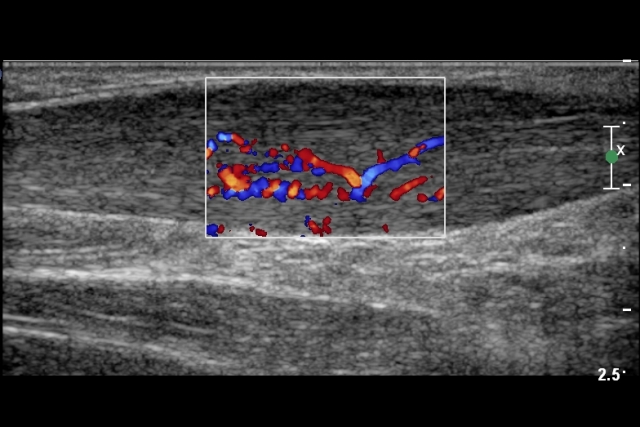

Example of ultrasound microvascular swelling. Source. || MRI of Achilles Tendonitis. Source.
As you can see, this current “process” of tendinopathy involves a reactive and then degeneration response of the tendon through various stages leading to larger and larger disruptions in the tendon. Signs and symptoms of disruption such as pain, soreness, achiness, and so on typically increases the symptoms (but not always).
The “repair process” arrow going up is progressively less filled in. From current research we know that a tendon in a state of reactive tendinopathy can repair well back to normal tendon structure. However, as you move into tendon dysrepair classification, the ability to repair such tissue decreases as you get more severe. What ends up happening instead is that scar tissue develops which is much less strong than normal tendon tissue because of the type of collagen (type III collagen instead of type I) and orientation of the collagen structure (scar tissue is haphazard collagen deposition instead of parallel alignment which is stronger) or apoptosis occurs and there is a lack of collagen in the degenerative area.
These “stages” are not exactly discrete and able to be diagnosed accurately except with medical imaging techniques. These stages progressively move into one another, so there’s no time where you may only be in one stage and then immediately go to another stage. It’s most likely that you will be between stages of normal and reactive tendinpathy or between stages of reactive tendinopathy and tendon dysrepair. A trained medical professional may be able to give a diagnostic analysis of where you likely are according to the presentation of signs and symptoms and reaction to training.
General signs and symptoms of moving from reactive tendinopathy to degenerative changes:
- Total rest does not work
- The tendon is stiff, achy, or sore after periods of inactivity such as after waking up
- You have chronically worked through signs and symptoms such as pain, achiness, soreness, stiffness, and so on for longer than 3+ months you may be at higher risk
Hence, it is important to remove offending exercises or intensities or loading and apply rehabilitation as soon as possible to stimulate the ailing tendon toward as much normalization of healthy tendon as possible.
Here’s an example of an illustration from the common flexor tendon from our illustrations with “reactive on degenerative tendinopathy.”
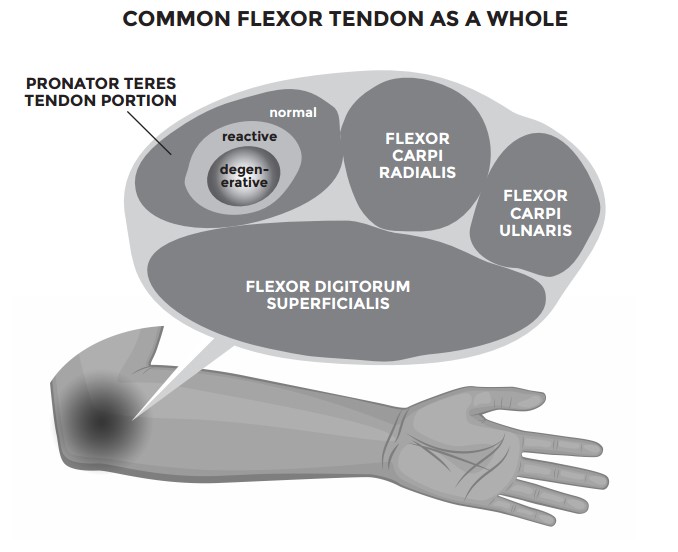
This image can be a little bit misleading in that there’s no actual “pronator teres tendon” in the common flexor bundle (as it all blends seamlessly into one), but the stress from the pronator teres muscle into the common flexor area can become degenerative and reactive if that type of movement is bothering you more than others. You commonly see more pronator teres area tendinopathy in climbers and gymnasts than say in golfer’s elbow.
In this example of golfer’s elbow, you should do all the rehab exercises:
- Wrist curls + eccentric — Flexor carpi radialis and ulnaris (FCR/FCU)
- DB or hammer Pronation + supination — Pronator teres
- Finger rolls/finger curls — Flexor digitorum superficialis (FDS)
Handbalancers and climbers tend to get more pronator teres or FDS area golfer’s rather than FCR or FCU which is why if they only do Wrist curls for rehab it may not improve that much.
It is important to understand that most tendons, even if they are in a degenerative state, can be rehabbed to be able to perform at a high level of performance. Tendinopathy does not affect the whole tendon. It only affects a portion of it like in the Common Flexor tendon example above. Only the affected portion will be “degenerative” but it will still repair just not as strong as it it were healthy. A rehabbed degenerative tendon will still be able to be strengthened to a high level. Elite athletes get tendinopathy all the time and play at a high level. You’re fine if you get it rehabbed.
Jill Cook goes over this concept in this video. Basically, the cross sectional area of the tendon in normal non-dysfunction tendon is say 100% of area. However, a dysfunctional and painful tendon might have a say 5-10 or more percentage area of dysfunction. But since dysfunctional tendons are actually larger than the normal tendon, the studies have identified that dysfunctional tendons have more normal tendon tissue than even a normal tendon.
What this means that the tendon is still strong enough even with the dysfunction and pain. Thus, the goal of rehab is to build load tolerance in the painful and dysfunctional para-tendon and tendon areas.
Common places where tendonitis is easily developed are located at:
- Medial epicondylitis (inner elbow – Golfer’s elbow) which arises from excessive pulling exercises.
- Lateral epicondylitis (outer elbow – Tennis elbow) which arises from excessive extension of the wrist.
- Triceps tendonitis (elbow) which arise from excessive pushing exercises.
- Biceps tendonitis (elbow) which arise from excessive pulling exercises.
- Wrist tendonitis (wrist) which arise from overuse at the computer or in excess flexion/extension of the wrist.
- Patellar tendontis (patella/knee) which arise from overuse in running, plyometrics, or weightlifting.
- Hamstring tendonitis (knee) from overuse in running, plyometrics, or weightlifting.
- Achilles tendonitis (ankle) which arise from overuse in running, plyometrics, or weightlifting.
If you have sore joints or tendons that are starting to become sore, this is your body letting you know that you should back off from exercise. This indicates that those body parts are under excessive volume or repetitive strain that you cannot recover from.
Symptom Severity
There’s many different classifications of symptoms, but this tends to be the most common.
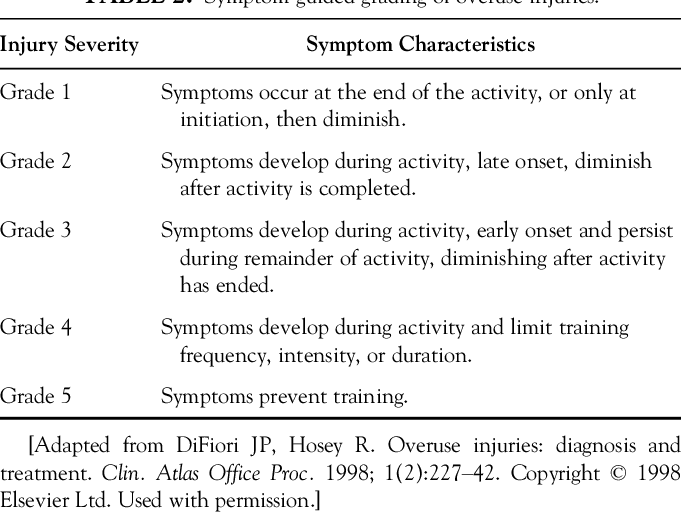
In general,
- Reactive tendinopathy tends to match with grade 1-3 and is considered mild overuse.
- Reactive to dysrepair tendinopathy tends to match with grade 3-5 and is considered moderate overuse.
- Degenerative tendinopathy tends to be deep into the grade 5 range for several months or longer.
No one should be really worried about degenerative tendinopathy unless they have been training through the pain for months or years. Most cases building load tolerance is going to help to get the reactive to dysrepair range to improve back to normal.
Common myths and misconceptions about tendinopathy rehabilitation
- Rest — You may encounter “rest” for tendinopathy as a common form of treatment from doctors, physical therapists, advice from others, and so on.
Rest typically only works in the range of normal tendon to reactive tendinopathy. It typically does not work for tendinopathy moving toward tendon dysrepair and degenerative tendinopathy stages. If resting does not help your tendinopathy, then it’s likely that there’s some dysrepair or degenerative aspects that need rehabilitation.
- Ice — not particularly useful. Compression is more useful for swelling. Blood flow does not need to be depressed below normal levels. Analgesics are more useful for pain. Some people have been having questions on this. Let me explain the reasoning.
If a tendon is in the reactive tendinopathy stage, then just rest will help if you wanted to just lay off it and let it heal. If the tendon is in a dysrepair or degenerative stage, then it’s “tendinosis” — there’s little to no inflammation present in the injured portion of the tendon. Since ice decreases inflammation, there’s no need for it since there’s no inflammation.
As you can see, there’s no need for ice either way.
- Analgesics — There was some debate about whether or not to use NSAIDs on any level for tendinopathy because they decrease inflammation, and inflammation is critical to the healing process. However, since there is limited to no inflammation, analgesics like NSAIDs don’t help with tendinopathy.
Generally, if you want pain relief I’d go with isometrics for pain management. Ask your doctor for more information.
- Pain — You may have heard that you shouldn’t push through painful exercises as pain is bad. This is false. The reality is that you shouldn’t push through aggravating exercises.
The difference between painful and aggravating is simple. Some exercises during the rehabilitation process may be painful, but they yield a positive result over the course of the next few sessions. These painful exercises are positive to the rehabilitation process. On the other hand, non-painful exercises may aggravate the tendon and lead toward more degeneration. Hence, it is best to remove aggravating exercises that lead to decreased performance, increased pain, and signs and symptoms of progressive tendinopathy.
Pain that is generally OK during rehab usually has all of these:
- < 2-3/10
- Does not get worse during the exercise
- Does not get worse after the exercise or the next day
- Improvement of strength and function by the next rehab session
- General decline of symptoms over time with the rehab
Of these the last 2 are generally the most important to consider, but typically all of them is the best indicator that someone is not doing rehab at a capacity where it’s unhelpful.
In general, appropriate loading (sometimes with painful exercises) leads to increases in function via strength and endurance. As the muscle and tendon function improves, pain usually goes away. Pain is generally correlative in an acute injury to an aggravating exercise, but not in a chronic injury (3-6+ months). Hence, why I tend to suggest painful rehabilitative exercises be only performed under qualified medical professional treatment. Do so at your own risk.
- Blood flow — another common misnomer of tendonitis is that increasing blood flow helps repair. I believed this previously, but research has shown that tendinpathy typically increases blood flow to the tendon while rehabilitation resolves the blood flow to normal. This is a bit confusing at first because it seems that increasing blood flow to the area would help with tendinopathy, but let’s look at things logically.
In tendinopathy, the affected tendon tends to swell and in some cases has angiogenesis/neurovascular in-growth (nerves and blood vessels growing into it) which is considered a failed healing response. Getting more blood to a failed healing response does not make it any better. If anything more blood to an area of swelling tends to exacerbate the swelling more than it would help similar to putting heat on a swollen sprained ankle. If you want to reduce swelling and normalize blood flow you’d use ice, but generally ice isn’t really indicated for sprained ankles now either unless it’s extremely severe which it balloons up.
Here’s another way to think of it. If blood flow was effective then just putting a heating pad on the tendon area multiple times a day should make it heal faster because heat brings a lot greater blood flow to the area. Heat inducing greater blood flow is scientifically proven. However, heat does not improve tendinopathy like that otherwise it would be effective in studies and a staple of tendinopathy rehab.
Voodoo flossing also falls under this as ineffective because of increased blood flow. It may be helpful or neutral as far as joint mobilization and potentially breaking chronic pain patterns.
Research on angiogenesis in tendinopathy for further reading.
I happen to like heat with the tendon, but it is not because it increases blood flow. I like it because it helps to decrease tendon stiffness and help to warm it up for rehabilitation exercise.
General summary of studies on tendinopathy
General summary of what works on Instagram:
- https://www.instagram.com/p/CfR2RHoOFK2/
- https://www.instagram.com/p/Cfz8Sv5u-mh/
The only thing in the scientific literature that has high quality evidence to support rehab in tendonitis currently is eccentrics. Everything else seems to be approximately no evidence to low evidence with a few things such as ECST (extracorporeal shockwave therapy) or PRP (platlet rich plasma) maybe being tentatively moderate evidence in lower body tendinopathies (although it varies).
- High quality evidence = multiple random controlled trials support it
- Moderate quality evidence = at least 1 random controlled trial supports use of it, with underlying scientific reasoning, case studies, and other non-RCTs.
- Low quality evidence = scientific reasoning, case studies, non-RCT studies support the use of it
- No evidence = Doesn’t work
- Conflicting evidence = studies don’t agree.
General summary of various things that work and don’t work:
- High quality evidence = eccentrics. This is likely the best study explaining why eccentrics work.
- Moderate quality evidence = ECST knee and achilles (moderate to weak),ECST for calcific tendonitis. Surgery (variable from low to moderate, and depends which surgery. Some have high satisfaction)
- Weak evidence / No evidence / Conflicting evidence = PRP (platelet rich plasma), PRP for knee (moderate to weak but need to be in conjunction with eccentrics, overall mixed results), LLLT (low level laser therapy — weak helpful, mainly for pain), ECST (covered above), prolotherapy and other sclerosing injections (probably helps, but still limited evidence), stretching and balance training (no evidence or make it worse — hence why I only use stretching for range of motion deficits), massage/manual therapy (case studies weak evidence in support, systematic reviews helpful in conjunction with eccentrics), acupuncture (might help lower body), dry needling (little to no evidence), possible improvement with nitroglycerin, ergonomics (useful for pain management, but doesn’t solve the problem), supplements like fish oil, gelatin, vitamin C, L-lysine, glucosamine and chondroitin, (See bottom of this article for supplements section), etc.
- No evidence = Ultrasound (doesn’t work), NSAIDs (no evidence as tendinopathy is generally not inflammatory)
- Can help but too much makes it worse and possible long term issues = corticosteroids/cortisone (short term better pain and function, long term worse)
Notes: joelschopp mentions a few others: Myofascial release/ART one, two, three; LLLT may be improving as they determine better targeting and wavelength selection. esaul notes I forgot to addin nitroglycerin patches which seem to help improve pain and increase strength in the tendon but probably don’t fix the issue. Two.
Note 2: IASTM – instrument assisted soft tissue mobilization supposedly aims at breaking down scar tissue (including Graston). IASTM seems to be OK for short term increases in range of motion but not much else. ASTYM – augmented soft tissue mobilization supposedly aims at increasing the body’s regenerative processes. Supposedly. ASTYM may be assist or help along with eccentric exercise in tendinopathies. Needs more high quality studies. Though evidence is still emerging. Worth a shot, if traditional stuff has failed.
Therefore, the primary exercise(s) are based off of only eccentrics. The peripheral work that may help is simply other comprehensive things you can do that won’t hurt but may help due to the range of no evidence to low quality evidence that is the rest of the treatments. There may be some placebo effect involved, but who cares if you’re getting better. The reason why I grouped weak evidence to no evidence is that even if there was a potential beneficial effect, the effect is usually very low at most or it may work for pain but not actually the tendonitis. It’s hard to distinguish when there’s a lot of conflicting results.
Do you have potential tendinopathy and chronic pain?
I added this section since I’ve been getting a lot of questions on the reddit with long term tendinpathy cases.
Read this post on the difference between chronic pain and injury pain for the expanded version.
If you’ve had tendinopathy for several months to several years (e.g. usually 3+ months is considered to potentially be chronic pain), and the pain is staying the same with rehab, then you may have chronic pain. Chronic pain is not considered a death sentence or anything like that now.
There’s a lot of factors that go into pain (biopsychosocial model for instance), but we can understand chronic pain as a dysfunction of the pain system. Pain, especially chronic pain, is not correlated at all with any damage to the tissues. What usually happens is that you get injured and/or have tons of repetitive movements, the nervous system may start to sensitize itself to the pain pattern usually by working through the pain and continuing to exercise. This means that it takes a lower and lower stimulus to cause the pain to happen. Thus, normal movements that may not have caused pain before may start having a painful feeling with them. In other words, normal movements that would not have normally caused any pain may start to have pain with them. The nervous system built a “bad habit” by creating a pain pattern with particular movements.
This is common in tendinopathy and other injuries when an athlete or patient has rested for several weeks but the pain remains constant or still there. The nervous system has been sensitized to the pain stimulus, so normal movements are causing pain when they are not supposed to. The reason why it’s likely chronic pain is that if you rested for several weeks or longer is that the tissues themselves have had time to heal fully, which means that there is no tissue damage but the painful sensations are continually there. This is especially apparent when very light movements such as Achilles calf raises or DB wrist curls with light weights such as < 3-5 lbs are causing pain. These would not normally cause pain or be difficult even in a sedentary population, so if everything is healed why would they be causing you pain? They shouldn’t, and that’s one of the big reasons why we know we’re working with chronic pain rather than anything with any tissue injury.
Generally speaking, chronic pain rehab works on improving strength and function but also includes several methods to start to desensitize the nervous system such as:
- Proper pain neuroscience education (PNE in the scientific literature)
- Graded exercise exposure (acclimate the body to consistent exercise + endorphins)
- Relaxation exercises (desensitize the nervous system)
- Novel movements (demonstrate to the nervous system that normal movements with the area don’t cause pain which desensitizes it)
- Sensory and sensory discrimination exercises
- Cognitive behavioral therapy
And potentially other stuff as well. If you suspect you have chronic pain, only doing rehab stuff below will almost always not work just like most traditional physical therapy and other interventions usually fail. In my practice, I typically use relaxation, novel movements, and pain education to start and then bring in some others if the chronic/persistent pain is being stubborn.
My advice would be to see a physical therapist that has experience with chronic pain patients. If not, you can post on reddit and/or check out the consults page. These vids helps to explain things well.
Edit — I’ve recently gotten a bunch of questions about RSI (repetitive strain injury) as it relates to Tendonitis/Tendinopathy and chronic pain. You can read more about that here:
- https://www.reddit.com/r/overcominggravity/comments/jywwjv/question_about_the_difference_between_reactive/
- https://www.reddit.com/r/overcominggravity/comments/k4g52m/2_years_chronic_hand_pain_not_sure_which/
- https://www.reddit.com/r/overcominggravity/comments/k0zzrk/will_my_hands_ever_be_normal/
- https://www.reddit.com/r/overcominggravity/comments/k7icrs/chronic_pain_questions/
- https://www.reddit.com/r/overcominggravity/comments/kahfj6/tennis_elbow_rehab_update_plus_further_questions/
With this being said, there are some newer techniques that have garnered some support in the scientific literature like Percutaneous Ultrasonic Tenotomy (PUT). If there is a large amount of potential “damage” to the tendon on MRI, this procedure can remove the potential damaged tendon and does provide some symptom relief to a large amount of the people who have it.
On the other hand, I have done chronic pain PT with many people who have had it for years, and damage on MRI or ultrasound does not mean someone cannot have damage on imaging and be pain free again. There are numerous MRI studies showing that people with no pain or dysfunction have a lot of damage to their low back, joints, and tendons without pain or symptoms.
I’d generally recommend people do chronic pain PT first, but if someone wants to try PUT and they have access then it can be a solid option if chronic pain PT is not working as effectively.
Corrective measures
General overview of all of this in my 2 Instagram posts:
Full range of motion concentrics + eccentrics — The only high quality evidence for rehabilitation
Research note: Heavy slow resistance (HSR) is a protocol that has gained a bunch of popularity in the past 5 or so years which seems to be effective for lower body tendonitis (achilles and patellar specifically). In this, you aim to do 3 sets of 10-15 reps with heavier weights and a slow eccentric phase. This has been proven to work for around 60-80ish% of the population with those tendinopathies as well, so if you want to use a scientifically proven method for lower body tendinopathies you can try this. If that doesn’t work, the higher reps protocol has had some success with non-responders of HSR. Likewise, the opposite: if you’ve tried higher reps and not tried HSR then HSR might work for you.
This is my take on eccentrics with a higher repetition phase and lighter weights which I have found to work in my athletes (primarily gymnasts and climbers) at about the same ratios. Choose HSR to start if you want to go by the research, but you can use higher repetitions effectively too.
- Do an exercise that works the muscles and tendon in question. So medial epicondylitis you do wrist curls, biceps you do biceps curls, Achilles you do calf raises, etc.
- 20-30 reps for 3 sets. Start at 30 and work your way up to 50 slowly. If higher reps make it worse after a few sessions then drop back down. Working through pain is fine, according to the scientific literature as long as function is improving. Rep ranges of 10-15, 30-50, and sometimes even 5-10 can work depending on circumstances.
- Not to failure on the reps. This is super duper important as going to failure is when most people re-injure themselves!!
- 2s uniformly slow controlled eccentric and 1 seconds concentric. For example, 2010 tempo works. Basically, controlled is the name of the game. (I initially recommend 3-5s eccentrics, but that tends to take too long for most people so 2-3 is similar and cuts half the time).
- 3x a week frequency. Can go up to 4x a week if it helps. If it doesn’t help drop back down.
If one does not work, then try the other. I’ve seen multiple cases where high repetitions didn’t work but HSR did, but if HSR didn’t work the higher repetitions do. I suspect this might be due to the stage of tendinopathy: the tendon dysrepair stage might benefit from a lighter stimulus of high repetitions whereas if the tendinopathy is particularly bad such as the degenerative tendinopathy stage it may benefit from heavier repetitions to stimulate healing. This is only my hypothesis.
The majority of the achilles and patellar studies showed that working through pain was fine during eccentrics rehabilitation. However, be smart about it: if working through pain ends up aggravating it — the tendinpathy is getting worse over sessions instead of better — then don’t keep doing it.
Should you only do the eccentric and not the concentric?
Literature reviews like this one suggest there is no consensus about only doing the eccentric portion.
Synopsis Tendinopathy is a very common disorder in both recreational and elite athletes. Many individuals have recurrent symptoms that lead to chronic conditions and termination of sports activity. Exercise has become a popular and somewhat efficacious treatment regime, and in particular isolated eccentric exercise has been promoted. In this review we cover the relevant evidence for different exercise regimes in tendinopathy rehabilitation with particular focus on the applied loads that are experienced by the tendon and how the exercise regime may affect these applied loads. There is no convincing clinical evidence that demonstrate that isolated eccentric loading exercises improve the clinical outcome more than other loading therapies. However, the great variation and sometimes insufficient reporting of details of treatment protocols hamper the interpretation of what may be the optimal exercise regime with respect to parameters like load magnitude, speed of movement, and recovery period between exercise sessions. Future studies should control for these loading parameters, evaluate various exercise dosages, and also think beyond isolated eccentric exercises to arrive at firm recommendations regarding rehabilitation of individuals with tendinopathies.
Also, this study:
Results — The eccentric-concentric training combined with isomentric contractions produced the largest effect in the reduction of pain and improvement of function at the end of the treatment (P < .05) and at any of the follow-up time points (P < .05).
Conclusion — The eccentric-concentric training combined with isomentric contractions was the most effective treatment. Future well-designed studies are needed to confirm the results of the present trial.
In general, this seems to make sense: when getting back to daily activity or sport you want to be training both the eccentric movement for the tendinopathy along with the concentric movement so you can properly and smoothly control the muscle action in both direction.
General exercises for eccentrics
Since some people were having difficulty with understanding what type of exercises are recommended for eccentrics, I’m showing some of the videos off of YouTube that represent these.
Rotator cuff:
Note: The supraspinatus can be particular difficult to hit. The first two videos are for the supraspinatus with DBs and bands. Can also do the a slow eccentric “empty can” test with only arm weight and move to light DBs as rehab progresses (third video). The last couple videos are ways to do infraspinatus eccentrics with bands and DBs.
In general, if the rotator cuff tendinopathy is diagnosed, I still recommended doing eccentrics for all of the parts of the rotator cuff so as to make sure that none are a weak link and that they’re all getting worked. Eccentrics will also strengthen the muscles and teach solid neuromuscular control as well, so you’re more likely to not impinge when fatigued.
Medial epicondylitis (inner elbow – Golfer’s elbow, climber’s elbow, etc.):
- Update – Medial elbow (golfer’s elbow, climber’s elbow, etc) 8-12 week Video Rehab Program has been released if you are interested in working with me to resolve your issues and get back to your sport.
See my Instagram series:
- Part 1: 3 Main Rehabilitation Exercises & tips – https://www.instagram.com/p/CgS-xDmA3f2/
- Part 2: Stretching and mobilizations – https://www.instagram.com/p/CglBrBpDSXs/
- Part 3: Massage and other soft tissue work – https://www.instagram.com/p/ChLqKR_gv2H/
- Part 4: Peripheral exercises that can help – https://www.instagram.com/p/ChvJaR7glPV/
This stretch (video version) helps a small portion of people too. This would be a case of a primary joint mobility issue that is putting excessive strain on the tendon or areas surrounding causing a secondary tendon issue. Variations of the finger roll/curl exercises — one and two.
As stated above, you should do all the 3 rehab exercises. Occasionally 4, but I usually start with 3.
- Wrist curls + eccentric — Flexor carpi radialis and ulnaris (FCR/FCU)
- DB or hammer Pronation + supination — Pronator teres
- Finger rolls/finger curls — Flexor digitorum superficialis (FDS)
- Ulnar deviation (occasionally needed) — Flexor carpi ulnaris
Handbalancers and climbers tend to get more pronator teres or FDS area golfer’s rather than FCR or FCU which is why if they only do Wrist curls for rehab it may not improve that much. The reason why you do all the rehab exercises is that you want to not only strength the reactive or degenerative portion of the affected tendon, but also preferentially strength the area(s) of the healthy tendon to bear load if the area(s) of the affected tendon are end stage degenerative. I’ve found that including all of the exercises tend to work the best.
Also, strengthen the shoulders/rotator cuffs for both medial and lateral can be helpful as if the upper chains are weak this can be problematic with more stress at the elbows. Face pulls are a good exercise if they don’t aggravate the elbows.
For medial and lateral epicondylitis (golfer’s and tennis elbow) the “Tyler Twist” flexbar can also work effectively.
Lateral epicondylitis (outer elbow – Tennis elbow):
Note: The video does not depict a slow eccentric.
For medial and lateral epicondylitis (golfer’s and tennis elbow) the “Tyler Twist” flexbar can also work effectively.
Triceps tendonitis (elbow):
Note: There’s quite a few ways to do this. Machines are one (triceps pushdowns). DBs are another and you can do them as seated (arm overhead triceps eccentrics), standing (arm overhead triceps eccentrics) or lying (skullcrushers). I only linked a couple, but you can YouTube the others.
Biceps tendonitis:
Proximal biceps:
Distal biceps – Any type of curls work.
I prefer light preacher curls to start with lockout at the end of range of motion if it is tolerated fine. If not, standing curls work. Play around with the hand orientation (supinated, hammer, or pronated) to find out which works best for you. Sometimes certain hand orientations bother the elbow (e.g. make it worse over time) than other configurations. You do not need to “feel” the area working for it to be effective for rehab nor does there need to be pain. I prefer painless exercises in most cases.
Note: The first exercise is for (proximal) long head biceps tendinopathy up at the shoulder, and the second exercise is for distal biceps tendinopathy down near the elbow.
Wrist tendonitis (wrist):
Depending where it is on the wrist, it may be the same as medial and lateral epicondylitis. However, I would suggest getting this checked out since there are different issues with the wrist that may present at tendinopathy, tenosynovitis, or other wrist issues that may not respond well to eccentrics.
This is the reason why I’m not linking a video, and the other is you can scroll up to the medial and lateral epicondylitis sections.
Rice bucket can also be effective for various wrist rehabilitation. I’ve seen it used effectively in practice with baseball players, gymnasts, traceurs (parkour), and climbers.
Achilles:
Note: This eccentric should be done on FLAT GROUND if you have insertional achilles tendonitis. If it is mid-portion achilles tendonitis, doing them on an elevated surface where you can drop your heel down below level is recommended.
Achilles tendonitis is the most studied in the literature, and here are the 3 most popular regimens in order of new to old.
- Silbernagel — http://www.raynersmale.com/blog/2015/10/22/treatment-of-achilles-tendinopathy-with-combined-loading-programs
- Alfredson — http://www.runnersworld.com/sweat-science/eccentric-calf-strengthening-for-achilles-tendinopathy-five-years-lat
- Curwin and Stanish — http://www.mincep.com/prod/groups/ump/@pub/@ump/documents/content/ump_content_421642.pdf
Patellar:
Note: A tilt board is most effective to isolate force onto the quad and patellar tendon. I would start with both legs instead of one leg, as starting on one leg can be too intense for some and aggravate the condition. Alternatively, seated knee extension eccentrics with a machine or ankle weights can be used to isolate instead.
Hamstring:
Note: There are several ways to do this, so find one that works for you. You can also use a band as well for this and patellar, if positioned at the right angles.
Peripheral work that may help:
- Remove the aggravating and offending exercise(s) by going down a progression or substituting them. Do not stop working out.
- If things are too painful isometrics can be useful at 70% to 80% (Note: 80% of 8 RM so probably around 50-60% 1 RM) of MVIC (maximum voluntary isometric contraction). In other words, put the joint(s) in neutral position and load it and hold for 5-10 seconds or until pain is reduced without moving the joint(s). This should be done before the rehab work to reduce any pain that may occur. You can also try Doomgoober’s slow MVIC movement.
- Light stretching for the agonists and antagonists (light stretch = slightly into discomfort). If this does not help, remove it.
- Heavy stretching, ONLY IF there is a range of motion deficit that needs to be corrected. For example, very inflexible forearms for a climber. Otherwise, stretching may aggravate a tendon, especially in the dysrepair or degenerative stage.
- Soft tissue work or massage to the affected muscle — a bit to the tendon itself is OK but it can aggravate it in some cases. Aim to loosen any knots or tight spots in the muscle which may be putting tension on the tendon at rest.
- Strengthening to the antagonists (so if it’s biceps tendon, strengthen the triceps. Forearm flexors then do forearm extenstor work, achilles then do some anterior tibialis strengthening). Eliminating imbalances that can be a potential risk factor and maybe cause are a good idea.
- Mobility work throughout the day non-painfully
- Heat can be useful. Don’t use ice (or RICE protocol). Analgesia is better for pain than ice, and compression is better than ice for swelling. No reason to use ice. MEAT — movement, exercise, analgesia, treatment — is better.
If there are options that I have not covered here, let me know.
Planning rehabilitative sessions
Integration with regular workouts is the same. Do your workouts, then the structure suggested above. If the workouts require use of the injured limb and does not aggravate it, then make sure the tissue is sufficiently warmed up before doing anything.
Proper structuring of the modalities listed above is important. Here’s the combination of things that I’ve found work the best.
Ordering of rehab/prehab:
- Heat and/or mobility to warm up
- Soft tissue work, if wanted
- Light stretching
- Strengthening with agonists and antagonists including the sets of 30-50+ not-to-failure exercises with the 3-5s eccentric.
- If you need more range of motion then flexibility work if needed
- Follow up with mobility work, especially if there is new range of motion from the flexibility work
Eccentrics (agonist work) is performed 3-4x per week. The rest such as mobility, soft tissue massage, heat, and so on can be performed 5-7 times per week. If the rest of the peripheral work makes it feel and perform better with higher frequency, feel free to do so.
Source. It’s generally best to do main rehabilitative exercises 3-4x a week, since you get net tendon synthesis only between about 36-72 hour window. The degradation outweighs the net synthesis for the first 0-36 hours approximate.
Remember, having an injury where you need to add in prehabilitative work doesn’t mean that you should rest everything and neglect other training. If you have medial epicondylitis (elbow tendonitis) for example you can still do legs and core work as well as do other skill work for your sport and corrective nature things such as flexibility/mobility.
One of the big things with tendonitis at “stability” joints such as the elbows is that there tends to be a loss of mobility in the wrists and shoulders thus putting more stress on the elbows. The same thing occurs with tendonitis at the knees and losses of mobility at the ankles and hips. Thus, if you have tendonitis at the elbows or knees you should work on improving the strength, flexibility, and mobility of the two joints surrounding it.
Here’s some general phases of the rehabilitation process.
2015 Malliares et al study on process of rehabilitation
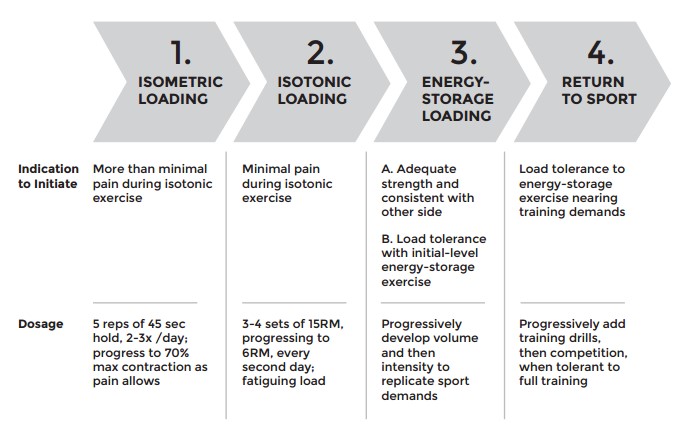
2018 Mascaro et al systemic graded approach
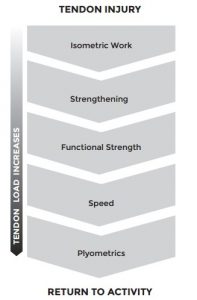
Both of these work, although Mascaro et al has a couple more phases to it by introducing a strengthening to functional strength to speed to plyometrics. This generally means isolation -> compound movements -> slowly increasing the speed of movements -> explosive loading of the movements. Mascaro’s is probably superior slightly because going too quickly to energy storage can increase risk of reinjury.
Getting back to exercise
Acute cases: I generally recommend start with 40% intensity or so and ramping back up about 10-15% intensity and volume of the workouts every week. So it may take about 2-6 weeks to get back into your regular workouts, depending on how bad the tendonitis was before. Longer if it was more severe.
Generally speaking, whether you use heavy slow resistance or higher repetitions, I always recommend working back into various weighted exercises and progressions with high repetitions. Start out within the 15-20 range before ramping down into the 5-12 range for strength and hypertrophy. Slowly go down about 2-3 repetitions per week.
If you’re in the reactive tendinopathy stage and just rest lets it normalize then you’ll want to work back into it over 2-3ish weeks. Tendon dyrepair will take 3-6ish weeks. The degenerative tendinopathy stage will tend to take anywhere from 5-6+ weeks most likely. Usually the latter two stages will need to be played by feel depending on how your tendon is responding to the intensity, volume, and load of exercises. Don’t be afraid to back off if it’s being aggravated.
Chronic cases: If rest doesn’t work, and you’re in the reactive on degenerative or tendon dysrepair stage, then you may have to go more conservative. In this case, I tend to recommend starting with about 20-30% of volume, and work your way up by increasing about 5-10% volume per week.
The key here is NOT pain. It’s likely that there may be pain during the rehabilitation process if there is any degenerative tendon. Instead, the key here is to look for progress on loading and decreasing the pain as the rehab process continues. I generally do not recommend increasing the weights every workout in this case. Rather, you may stick with the same eccentrics for 1-3 workouts in order to allow the body to accommodate to the volume.
Overall, acute cases tend to take about the 2-6 week window I mentioned before. Chronic cases tend to take anywhere from about 4 weeks up to 3 or more months. If the case is extremely severe, it may take 5-6+ months. As an estimate, for every month (4 weeks) you’ve had it, it tends to take about 2 weeks of consistent rehabilitation to get back to normal activity. IF you don’t keep aggravating it during workouts. If you’re an athlete, it heavily depends on your schedule.
For my patients and clients, I like to keep very high repetition isolation work in someone’s routine for another 1-2 months after they have fulled recovered and are back to normal activity. For example, if you had biceps tendinopathy, you should continue to keep doing high-repetition, not-to-failure sets of biceps curls such as 3 sets of 30 repetitions.
Remember, pure rest doesn’t work unless you are in the reactive stage. Don’t do pure rest. Always do some sort of prehabilitation or rehabilitation work.
This is simply a general guideline and your case may vary. Talk to a qualified medical professional before using any of this information because it is not tailored to your specific case.
Overcoming Tendonitis is difficult but it can be done successfully.
Should I work through the pain during rehabilitation?
Generally, I have 2 different progressions I use for pain.
- Someone can go into mild pain 0-3/10 as long as they’re improving in strength and function from session to session AND symptoms are decreasing over time. In this case, symptoms can be there during a session or after a session but are OK as long as the 2 criteria are met. This is generally a positive progression because you’re building the load tolerance over time with increasing strength and function and symptoms are going away.
- If someone has a very irritable tendon, chronic pain, or other type of injury, I recommend not going into any pain or types of symptoms because that generally tends to be too aggressive of a protocol for load management or in the case of chronic or persistent pain can reinforce the pain pattern that you are trying to eliminate. This is generally not because you’re re-injuring your body or anything like that but because the irritable tissues (or chronic pain as well) means your strength and function are generally trending in a backward progression.
In general, progression 1 is mainly for people who have a very simple and straight forward cases where you can progress rehab pretty easily. Progression 2 tends to be for those with chronic or persistent pain where the pain pattern is being activated consistently with exercises that would not normally cause pain in most other people or if you have a very irritable tendon where rapid progression can easily cause reappearance of symptoms. In most of these cases, pain education is very important and distinguishing between a chronic pain case and a very irritable tendon case is important for progression. It can be some of both sometimes.
Should you continue your sport(s) while doing rehabilitation?
The brief answer is yes.
There are numerous reasons which are detailed in these posts:
Generally speaking, do as much sports specific movement as you can without aggravating the injure(d) areas which will make it worse. Pain is not always an indicator of worsening an injury, especially during the rehabilitation process. You do not want your body to de-condition and atrophy by taking time off from your sports.
It’s best to consult with an orthopedic doc or physical therapist who works with athletes in you particular sport or discipline to find out what they recommend or tend to see works well for their patients with similar injuries.
Doing non-painful sports activities is a decent rule of thumb, BUT it is not always the case that it works so just be aware of that. If an injury is getting worse even with non-painful sports specific activities, then you may want to lay off and get it checked out.
Braces and equipment
Braces do NOT fix the problem, but they can be an effective tool for pain management while you rehabilitate an injury (under the proper supervision of a medical professional). Here are some pictures of braces that are effective for pain management of various conditions.
Clicking the image will take you to it.
Lateral and medial epicondylitis
The smaller area-specific braces help with pain management. There are sleeve-type braces that may also be effective, but from what I’ve seen in real life the smaller ones you can compress around the area tend to be the most effective for pain alleviation. Two examples are above.
Research for medical epicondylitis is virtually non-existent. Research on lateral epicondylitis is depressing, as some treatments work short term for pain and function but are long term ineffective. It goes away on it’s own in some people.
Wrist tendonitis
Generally, wrist braces suck because it’s hard to find one that fits really well. If you have tendonitis and need to limit mobility and add some stability, ACE wraps or any type of elastic wrap works fine.
Triceps tendonitis — Compression bracing may help. Something like this may work, but sizing is a big issue.
Shoulder tendonitis — No bracing really helps. Be aware of posture/alignment and scapular mechanics.
Knee braces
Like the elbow, the knee straps that are more effective for pain management are the smaller ones. You can try sleeves if you want, but I don’t think they work as well.
Achilles tendonitis
Compression bracing may be more effective for achilles than other areas, probably because there’s a lot of interaction between the muscles of the foot and how the ankle functions. This is why calf stretching is integral to improving plantar fasciitis, because the superficial posterior (back) line of fascial goes all the way from the back down the leg and into the foot. Remember that this doesn’t solve the issue, contrary to popular belief of easy fixes.
Other equipment
Soft tissue devices where you can compress the muscles and massage them can be effective in some cases if you need myofascial release and/or trigger points that cause a lot of tension on the affected tendon. Loosening these tight muscles can provide instant relief in some cases.
Regarding the supplements that may help
Research note: As of the Overcoming Tendonitis book, we do NOT recommend any supplements because there is not enough information to accurately say that anything helps. But I’ll leave the list up so you can try some if you really want.
- Fish oil — Maybe but trending unlikely. Essential fatty acids and anti-oxidants helped and didn’t help. The latter is hard to say because almost nothing works for lateral epicondylitis in the long run and it resolves by itself in many cases.
Carlson’s fish oil is one I have used before. High DHA/EPA content. Doesn’t taste nasty.
- Gelatin — May help. Gelatin has collagen in it, and hence can potentially be used for tendon repair. Cartilage too. This is especially true since the body cannot make all of the needs of collagen production itself. Vitamin C enriched gelatin improves collagen production in vitro. Take pre- and post-exercise.
Knox unflavored gelatin is solid. Add it to your food/drinks. Jello works as well.
Naterman’s anecdotal evidence on gelatin + vitamin C combo with resistance training timing.
- Vitamin C, L-Lysine, hyaluronic acid — also components of tendons like gelatin. Hyaluronic acid has research. Vitamin C enriched gelatin improves collagen production in vitro. Another and another. Seems more effective in tendon surgery than tendinopathies, but may help. I haven’t seen any studies on all of the components put together supplemented, but you can try it if you want.
- Glucosamine/Chondroitin/MSM — unknown. Athlete hearsay at this point.
Here’s a solid one if you want to try it.
- BPC 157 — I personally do not know much about this, but I’ve heard some anecdotes on it. Generally, based on the information we have on other injection therapies it’s likely a placebo effect if there is any benefit.
Probably talk to your doctor about this potential option.
This article was originally published August 19, 2009 on Eat Move Improve. Updated Dec 2016. Exercises and more information added March 2017. Full update January 1 2020 after the book has been released. Last updated May 2023.
Need more help?
- Injury Consultations if you want to work with me personally.
- Buy Overcoming Tendonitis: A Systematic Approach to the Evidence-Based Treatment of Tendinopathy or digital edition.
- Medial elbow (golfer’s elbow, climber’s elbow, etc) 8-12 week Video Rehab Program has been released too. Aiming to get more out for all areas of the body.
Questions about articles may be addressed to the Overcoming Gravity reddit.
Disclaimer: Any information contained on this site should not be misconstrued as professional medical advice. Always consult your appropriate medical professional before using such information. Use of any information is at your own risk.
I may earn a small commission for my recommendation and/or link to any products or services from this website. Your purchase helps support my work on education on health and fitness. See also: Full disclosure of site terms and conditions.
Author: Steven Low
Steven Low is the author of Overcoming Gravity: A Systematic Approach to Gymnastics and Bodyweight Strength (Second Edition), Overcoming Poor Posture, Overcoming Tendonitis, and Overcoming Gravity Advanced Programming. He is a former gymnast who has performed with and coached the exhibitional gymnastics troupe, Gymkana. Steven has a Bachelor of Science in Biochemistry from the University of Maryland College Park, and his Doctorate of Physical Therapy from the University of Maryland Baltimore. Steven is a Senior trainer for Dragon Door’s Progressive Calisthenics Certification (PCC). He has also spent thousands of hours independently researching the scientific foundations of health, fitness and nutrition and is able to provide many insights into practical care for injuries. His training is varied and intense with a focus on gymnastics, parkour, rock climbing, and sprinting. Digital copies of the books are available in the store.








