I’m continuously getting questions about the difference between chronic pain (also called persistent pain) versus regular pain. Here’s an expanded explanation from the part in the middle of the tendinopathy article.
What is chronic pain — the smoke alarm analogy
Chronic pain is essentially a dysfunction of the pain system of the body. A good analogy is cooking and a smoke detector.
Normally, a smoke detector sounds an alarm if there’s smoke when something goes wrong cooking. This can be considered a normal injury such as a sprained ankle. However, the smoke detector can malfunction to where it starts to go off at the wrong times and in many different manners. Here are three common ones.
- Smoke detector goes off with cooking movements — chronic pain only with specific movements. Repetitive strain injury (RSI) pain that comes on from small movements all the time even with rest tends to be a subset of this.
- Smoke detector goes off with hot temperature but no smoke — pain starts in one area such as the wrist with an exercise but not on the opposite limb. A lower pain threshold makes the area more sensitive and your body perceives it as pain.
- If the smoke detector goes off all the time — if you have pain all the time. The threshold for pain is lowered and lowered until there is pain all the time. How does this happen? If you push a finger into your arm it takes pretty hard pressure to feel pain, but if you push your finger into an area that is highly sensitive due to an injury like an ankle sprain it takes much less pressure to elicit pain. Now imagine if the nervous system is hyper-sensitive due to lots of potential factors (previous acute injury, high stress or anxiety, fear avoidance over pain, etc.) and you can get cases where even touching someone gently can cause pain or someone can have pain all the time!
There’s other potential cases, but this summarizes most of the common ones you see.
Two more important points:
- The difference is that unlike acute injuries or overuse injuries the dysfunction is with the nervous system (pain system) and not the body. In many cases of chronic pain, there is nothing wrong biologically with the body at all as the injury has healed.
- One can both have acute and chronic pain. One can have an acute injury to the musculoskeletal system, but also have a disproportionate pain to that injury due to a dysfunction of the nervous system. Many of the people I see with chronic pain may still have some acute injury, but there are varying percentages to the pain responses. 0-100% with the injury, and 0-100% with the nervous system. Can be 0% and 100% or 100% and 0%. Can even be 30:30, 50:50, 70:70, 0:70, 30:100, and so on.
- If you’re reading this after I suggested you may have chronic pain, it simply means that I think you have some degree of nervous system dysfunction that is contributing to an enhanced pain response. Again, one can have mostly acute pain and a bit of chronic or even moderate to high amounts of both.
This vid explains it in a different way with the “volume knob” analogy if this section was a bit confusing or you are a visual and auditory learner (5-6 mins).
How does chronic pain develop?
Chronic pain tends to develop after an injury and working through the pain and/or having to do repetitive motions over time. The nervous system starts to get “sensitive” (sensitization in the scientific literature) to having the pain occur during specific movements. Thus, the nervous system starts to ingrain pain as a ‘habit’ with the particular movements, and it becomes normalized. Unfortunately, pain during the movement becomes the new normal.
Pain is now associated with the movement and can become more sensitized such that you have it only with those specific movements, or even start to spread in some cases, or the most annoying one of all which is the pain is present all the time. I’ve had several chronic pain cases where the nervous system got so sensitized that they started developing pain all over their body.
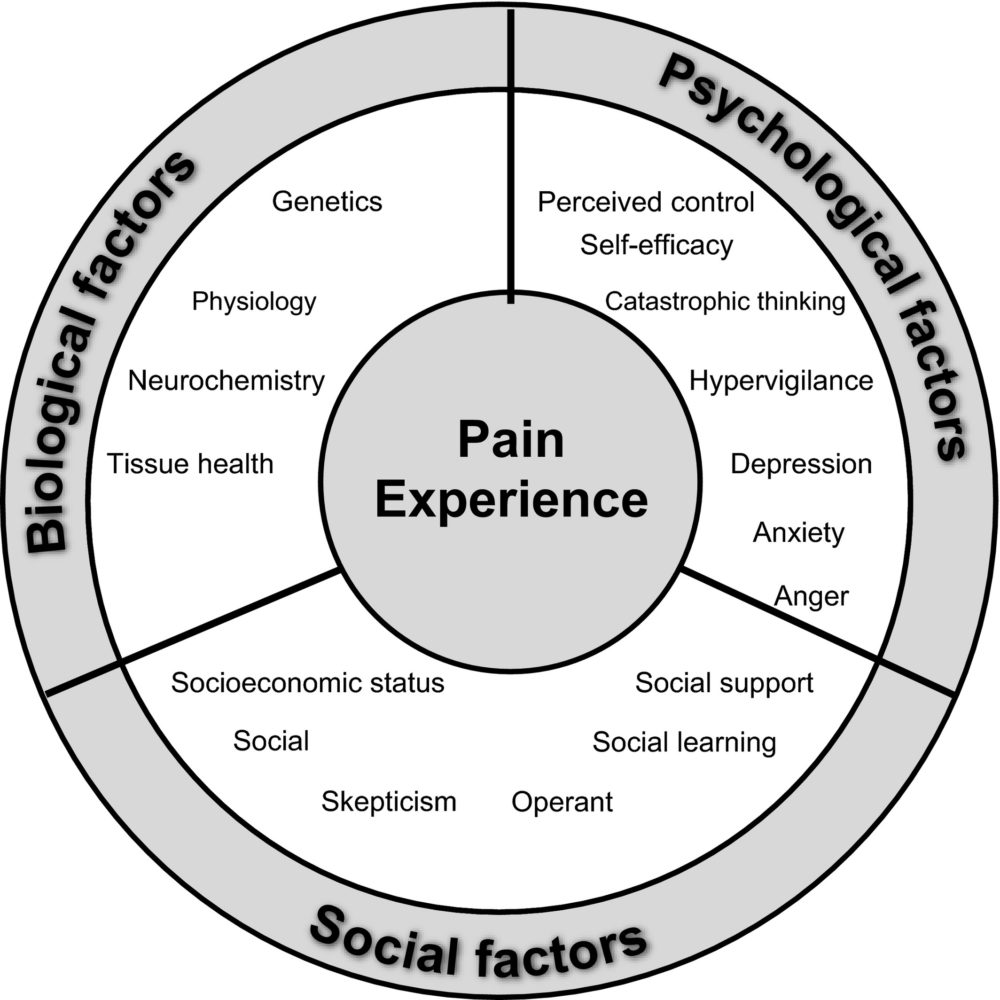
Since pain sensations — biopyschosocial model of pain — are affected by many different things things other than biology such as your psychological and social states can affect pain. Someone who is under a lot of stress, worry, fear, or has many negative thoughts about pain will generally have their pain intensify and worsen. This contributes to the increased sensitivity of the nervous system as well. Generally, also it’s common for people with pain to stop doing activities or social events they enjoy because of the negative experience of pain and this can also contribute to their pain worsening. All these factors can lead to worsening dysfunction of the pain system.
Our body does this through a process called Pain NeuroTags.
Essentially, when there is a pain stimulus for a long enough period of time, the neurons in the brain can have multiple dysfunctional adaptations happen that can potentially increase pain. It’s like your brain has picked up a bad habit.
- Imprecision/smudging — when neurons processing pain signals get mixed up with the movement you have an association of pain with a movement. Video explanation
- Disinhibition — when neurons accidentally activate because they’ve been activated so much (e.g. working through pain) you can get pain with normal movements that would not necessarily cause pain
- Facilitation — The brain has high plasticity which means it is able to learn and adapt. Unfortunately, neurons that process pain can also ‘adapt’ to learn how to process pain more efficiently and faster which means it may start activating pain signals more readily.
- Sensitization — The neurons in the brain pick up smaller and smaller signals from the body telling it to have pain.
All of these can lead to the process of developing chronic pain. Usually in some combination of each other.
What is the difference between chronic pain and normal pain?
The 3 month mark tends to be a bit indicator for when chronic pain is said to develop. At this point beyond any physical injury the body would have healed completely. For instance, if you sprain your ankle it’s going to be almost completely healed after a month or two. Even catastrophic injuries such as tendon or ligament ruptures for the most part after surgery have healed completely by about the 3-4 month mark, although rehab back to full strength and power might take longer.
If someone is still having pain beyond the 3 month mark, it’s unlikely for it to be related to any sort of damage to your biological tissues unless someone is pushing through vigorous activity or constant work activities that can aggravate the symptoms in a manner that may still damage tissues.
It’s common for symptoms to pop up during rehab, but these things are not an indication of setbacks and one should not worry about these. Rehab loads are very unlikely to cause any type of injury. They’re weights any sedentary or untrained person can use. What is happening is if during the acute phase of injury or into chronic pain the nervous system is more sensitive so steady progression of the intensity or volume of the exercise can sometimes cause symptoms to appear much like delayed onset muscle soreness (DOMS) appears if you start to workout and get sore muscles.
Common markers of chronic pain.
- Persistent pain > 3 months, especially if one has rested or been doing rehabilitation for prolonged periods of time. The injury(s) have completed healed by this time, so there’s no damaged tissues anymore which means the source of your pain is not your injury.
- Any imaging like MRI or diagnostic ultrasound with minimal to no signs of tissue injury while you are still experiencing a disproportionate amount of symptoms.
- Pain tends to activate or be intense with certain repetitive movements and especially movements that don’t involve heavier loading.
- Pain is common with everyday movements such as using a computer, phone, tablet, or everyday movements around the house
- A negative mental state where the patient ‘catastrophizes’ their pain with constant worrying, anxiety, fear, believing that something is wrong with their body, and losing hope the pain will never go away. This negative mental state actually increases pain symptom and makes it harder for rehab to work (“the general consistency of the findings highlights the potential role that PC – pain catastrophization – may play in delaying recovery from CMP – chronic musculoskeletal pain”).
- Pain intensity with rehabilitation workouts or other movements is generally out of proportion or highly variable in intensity even with very little to no changes in rehabilitation.
- There’s different variations of chronic pain. Chronic pain dispersed throughout the body is often due to central sensitization, while pain localized to a specific area or limb can be complex regional pain syndrome.
Generally symptoms are not something to base a rehab program around. What is more important is trends of increasing strength and function with trends of decreasing pain over time. Rehab sessions can and should be adjusted if the symptoms are too intense and interfering with good trend outcomes, but simply having symptoms does not mean anything is being injured or is wrong with a program or is a bad thing. It’s a normal thing.
What are the types of chronic pain interventions that are common to help rehabilitate chronic pain?
Now that you have a much better understanding of this topic, going back through the interventions listed in the tendinopathy article is much more helpful.
Generally speaking, chronic pain rehab works on improving strength and function but also includes several methods to start to desensitize the nervous system.
- Proper pain neuroscience education (PNE in the scientific literature) – This goes over a scientific article which can be helpful.
- Graded exercise exposure – acclimate the body to consistent exercise + endorphins
- Relaxation exercises – desensitize the nervous system. Typically, different types breathing, meditation, or other techniques. I use a combination.
- Novel movements – demonstrate to the nervous system that normal movements with the area don’t cause pain which desensitizes it
- Sensory and sensory discrimination exercises – reduce smudging and enhance the body’s mental map which helps to fix mixed up pain signals especially tied to certain movements (RSI, etc.), mirror therapy, and others.
- Cognitive behavioral therapy (CBT)
- Pain reprocessing therapy (PRT) – Examples – Somatic tracking, mindfulness, guided imagery, relaxation, emotional processing, etc.
Interestingly, they’re finding out hypersensitivity syndromes can be in all parts of the body. There is now identified visceral hypersensitivity syndrome which is not the same as inflammatory bowel syndrome (IBS) but is usually present with IBS that makes symptoms worse. The same is true of IBD and GERD. Gut directed hypotherapy (GDH) is one of the ways to treat IBS hypersensitivity. This is similar to chronic pain which uses CBT, sensory exercises, relaxation techniques, and others to help to calm down the overly sensitive nervous system.
There are others as well, but these are the common ones. Easily youtube or google-able if you wanted to know more information: Search terms: “[Insert intervention here] for chronic pain” such as “relaxation exercises for chronic pain.”
What should I do if I suspect chronic pain?
If you suspect you have chronic pain, only doing normal rehab physical therapy working on strengthening and other interventions usually fail. In my practice, I typically use relaxation, novel movements, and pain education to start and then bring in some others if the chronic/persistent pain is being stubborn.
- I do injury consultations and have worked with numerous people with chronic pain. I’ve had some people get rid of their pain in under a month (although this is more rarer), but most people it’s much longer and more gradual. Usually in the 2-4+ month range depending on the severity of symptoms and how efficient the nervous system is at activating the pain signals. We use the steps in the next section to start to desensitize the nervous system.
- Alternatively, call around to physical therapy clinics in your area, especially ones that work with athletes. You can call your local university or professional sports teams and ask who they use. Then you can call the clinics and see if they have anyone familiar with chronic pain rehabilitation and education on staff who can take your case.
If you’re reading this article you’ve probably tried to self rehab for months or years without success, or you’ve been through the gamut of many doctors, imaging such as X-rays and MRIs, and maybe even through several PTs and they can’t figure out what’s wrong. That’s because they were probably relying on the biological model of pain which does not work very well (or at all in some cases) for treating chronic pain.
Stop spinning your wheels or months or years or losing hope and despairing and get someone who is familiar with chronic pain/nervous system sensitivity who can help you.
A more in-depth video explaining the biological mechanisms and impact of how chronic pain develops and is treated (20 mins).
Any further questions can be directed to the reddit community.