THIS ARTICLE IS SCHEDULED FOR AN UPDATE IN JUN 2017
Introduction / To the top
Knee pain and injuries are common among weightlifters and even non-weightlifters. As I have discussed in Shoes, Sitting, and Lower Body Dysfunctions and many other articles, a lot of this stems from shoes and sitting and how they may have chronic detrimental effects on our bodies. Combine this with poor technique, especially in lifting objects off the ground or during working out, and you have a recipe for injury, pain, and inflammation.
This article is not going to be an end all article on how to solve knee pain and injury. Rather there are categories of knee injuries that all need different attention depending on what has been injured. From there we can determine what the best course of action that needs to be taken for each individual because everyone is a bit different.
This article is going to be relatively brief on each because there are many topics I will have to cover. I expect that if you have any questions they should be addressed to your orthopedic doctor or physical therapist. Searching the Internet or asking people on the web for more information is at your own risk.
Disclaimer: Any information contained herein is not professional medical or physical therapy advice. Always consult your doctor or physical therapist before using such information.
Categories of knee injuries / To the top
Knee injuries fall into a couple of categories depending on what types of tissue is injured, and the pathomechanics of how the injury develops.
Where the pain is occurring during movement is generally a good indicator of what may be wrong, and differential signs and symptoms can be used to further delineate what is wrong in most cases.

Image courtesy of Adam Inc. (though extremely modified)
Despite the generalized locations of what you think is injured compared to the chart sometimes the physiological issue or pain bleeds off into other areas. Also, there may be multiple pathologies in a certain area since there are a lot of different muscles, ligaments, tendons, etc. running through the area(s). I cannot say for sure (again, this is the Internet after all) that if you have a pain in a specific area that it corresponds to the conditions. Thus, for a sure diagnosis you should definitely see an orthopedic doctor or physical therapist on these issues.
Additionally, the pathology of knee injuries is very important. Often times for many of the types of non-impact knee injuries there are also mobility or flexibility issues at the ankles and hips. The knee sits smack dab in the middle of the two longest bones in the body, the femur and tibia. Given this alignment any issues in the ankles and hips that create any odd forces are distributed along the kinetic chain into the knees. Since the bones are so long any of the torques (Torque = Force * Distance) at the adjacent joints are magnified significantly which means that something as small as a bit of tightness in the ankles or hips can lead to a significant change in torques at the knee which may exacerbate or even create a pathology.

The knee is between the longest bones in the body // Photo from http://kitssportschiro.com
If there is a loss of range of motion at some joints, the other joints or tissues will have to take up the slack. This leads to many types of overuse or compensation injuries.
This means that in addition to any potential rehabilitation there needs to be an assessment of the whole lower body up to the back to ensure that things are moving correctly especially with recurring knee injuries. If you know you are tight or have a lack of mobility in certain planes this may also be your wake up call to eliminate tight areas. You may be surprised how much improving areas like the feet, ankles, hips, and back will improve your knee problems.
Notes:
1. If the pain is on the back of the knee then see the back of the knee section.
2. If the pain is over a particular muscle and not a tendon/ligament/connective tissue or deeper structure then see the muscle strains section.
3. If you suspect your injury does not fall into any of these categories then see the other pathologies section.
Given that you now know this head over to your particular section to see if we can possibly figure out what is going on with your particular pain and dysfunction.
Table of Contents
I. Introduction
II. Categories of knee injuries
III. Quadriceps tendonitis
IV. Patellar issues
V. Patellar tendonitis
VI. Tibial tuberosity issues
VII. Knee capsule / plica / medial collateral ligament
VIII. Pes anserinus issues
IX. Fibular head / biceps femoris / Lateral collateral ligament
X. Iliotibial Band issues
XI. ACL issues
XII. Meniscus issues (lateral and medial)
XIII. Muscle strains
XIV. The back of the knee
XV. Other pathologies
XVI. Conclusions
If you suspect you have an injury that does not fall into any of the categories above see a medical professional immediately. Also, if you have an injury which presents debilitating pain or presents possible insidious neurological symptoms such as sensory or motor deficits see a medical professional immediately. Motor deficits are critical enough that you may want to go to the ER ASAP.
Quadriceps tendonitis / To the top

Image from http://orthoinfo.aaos.org
Quadriceps tendonitis is one of the prototypical overuse injuries. However, this injury is more rare than patellar tendonitis unless the quadriceps muscles are (1) very tight and/or (2) have lots of scar tissue and/or (3) have biomechanical issues.
If you are quad dominant from sitting a lot with marginal activity (feel quads burning a lot while running, lifting, etc.) then this could be an issue that needs to be dealt with. Strengthening and activation work for the posterior chain and learning how to squat correctly will help a lot in the correction of this.
This is exacerbated more in women because they have a greater Q-angle which puts more torque on the knee. If you would like to read more about this you can see Shoes, Sitting, and Lower Body Dysfunctions which talks about this issue more in depth.

Photo from http://www.doctorkolstad.com/
Treatment
Thankfully, we have an article On Tendonitis for how to deal with both acute and chronic tendonitis injuries.
Remember, if the injury is acute then the treatment(s) that are most effective are RICE protocol, mobility work, light stretching, massage to the muscle, and potentially anti-inflammatories.
If the injury is more chronic then a protocol that work best are mobility, stretching, heat, friction massage to the tendon, massage to loosen up the muscles, and eccentric exercise. Eccentric exercise is one of the only proven non-invasive methods for rehabilitation of chronic tendonitis. This is the most important factor of a chronic tendonitis regime. See the above tendonitis link for more on this.
Learning how to squat correctly by engaging the posterior chain (glutes, hamstrings, etc.) will help significantly take stress off of this type of injury. So that is definitely one of the things that can be focused on aside from other modality treatment. Exercise should be focused on sitting back on the heels and not coming up onto the toes because that puts more stress on the anterior chain.
Patellar issues / To the top

Photo from http://www.kneeguru.co.uk/
Generally speaking, injuries to the patella or knee can need to be checked out by a doctor, especially if the pain is from an impact injury.
Around the patellar there are a myriad of structures. If the pain is around the quadriceps tendon insertion and patellar tendon origin then it may be related to those two overuse injuries respectively.
If the pain is slightly under the apex (bottom of the patella) that may be an issue with the infrapatellar fat pad.
If the pain is over the patella that may indicate overuse to one of the bursas in the area such as the pre-patellar bursa seen in the picture above, or just below the kneecap with a bursa such as the infrapatellar bursa (commonly referred to as clergyman’s knee).
Patellofemoral syndrome and/or chondromalacia patella is the other common cause of pain localized around the patella. These two often go together because they are somewhat coupled in the pathological etiology.
The knee is a delicate balance between forces that pull the patella laterally and medially, and it is just so happens that the muscles that pull it laterally tend to get more emphasized by poor biomechanics (e.g. inward collapsing knees during running, squatting, etc.) and are larger from the start. Vastus lateralis is bigger than the vastus medialis/vastue medial obliquus.
Now, what happens is that when the patella is start pulled more laterally is it starts rubbing on the lateral articular surface of the femur more and starts wearing down the cartilage both on the patalla and femur. This process starts softening and breaking down the cartilage (chondro = cartilage & malacia = softening) and will eventually cause a lot of pain and inflammation.
The reason why it does appear right away when this occurs is because cartilage has no sensory/pain fibers located within it. So only when it gets to a higher level of damage by wearing through a lot of cartilage and inflammation does your body start to feel the effects. This also means that there must be significant time taken to correct biomechanics because usually these are ingrained pretty well before the pain starts occurring so good care must be taken to teach proper technique especially with females who experience this issue.
Treatment
Typically, bursitis and fat pad irritation can be treated with typical RICE protocol, massage, and anti-inflammatories if necessary.
For the fat pad irritation if it is making the knee unstable taping can be an effective protocol to ensure that any mobility or exercise does not aggravate it any further.
Generally, for any impact injury to this area it should definitely be checked out by a doctor to make sure there is not any issues with the patella itself though.
With patellofemoral syndrome/chondromalacia patella there are multiple things we need to focus on. First, bringing down the pain and inflammation is paramount. Like the bursitis this can be done with the typical RICE protocol, massage, and anti-inflammatories if necessary.
Secondly, there must be loosening/strengthening of particular muscle groups. We want to strengthen the vastus medialis, vastus medialis obliquus, hamstrings, and glutes. We want to massage, trigger point, foam roll, tennis ball, etc. to loosen the vastus lateralis, rectus femoris, IT band, calves, hip flexors, etc.
Thirdly, we need to make sure there is enough range of motion at the ankles and hips. We want to especially gain more dorsiflexion in the ankles with calf stretches, and we would like to gain more hip extension by stretching the hip flexors as well as mobilizing hip internal and external rotation.
Many of the specific stretching/strengthening exercises can be found here.
Lastly, we need to teach proper biomechanics by deemphasizing the anterior chain by sitting back more in squats, teaching proper running technique, etc.
In addition, the knees must NOT be allowed to collapse in during any exercise that is taught. This is paramount. One of the best ways to do this is to cue to spread the floor with the feet during squatting, lunging, etc. if the knees want to collapse inwards. If this is ineffective, a band can be placed to pull the knees inwards to force the the person to think about forcing the knees outwards during the movement.
Since the glutes are one of the potent external rotators of the hip they should be evaluated for weakness/inactivation especially if there is a lot of sitting during the day. Once you get them active not only will it help correct the technique, but it will make you significantly stronger as well.
Patellar tendonitis / To the top

Photo from http://www.arthealthcare.com/
Like quadriceps tendonitis, patellar tendonitis is one of the prototypical overuse injuries. Commonly referred to as jumper’s knee this type of injury occurs often with lots of activity and improper biomechanical patterns.
If you are quad dominant from sitting a lot with marginal activity (feel quads burning a lot while running, lifting, etc.) then this could be an issue that needs to be dealt with. Strengthening and activation work for the posterior chain and learning how to squat correctly will help a lot in the correction of this.
This is exacerbated more in women because they have a greater Q-angle which puts more torque on the knee. If you would like to read more about this you can see Shoes, Sitting, and Lower Body Dysfunctions which talks about this issue more in depth.

Photo from http://www.doctorkolstad.com/
Treatment
Thankfully, we have an article On Tendonitis for how to deal with both acute and chronic tendonitis injuries.
Remember, if the injury is acute then the treatment(s) that are most effective are RICE protocol, mobility work, light stretching, massage to the muscle, and potentially anti-inflammatories.
If the injury is more chronic then a protocol that work best are mobility, stretching, heat, friction massage to the tendon, massage to loosen up the muscles, and eccentric exercise. Eccentric exercise is one of the only proven non-invasive methods for rehabilitation of chronic tendonitis. This is the most important factor of a chronic tendonitis regime. See the above tendonitis link for more on this.
Learning how to squat correctly by engaging the posterior chain (glutes, hamstrings, etc.) will help significantly take stress off of this type of injury. So that is definitely one of the things that can be focused on aside from other modality treatment. Exercise should be focused on sitting back on the heels and not coming up onto the toes because that puts more stress on the anterior chain.
Tibial tuberosity issues / To the top


Photos from http://www.boostphysio.com/ and http://4.bp.blogspot.com/
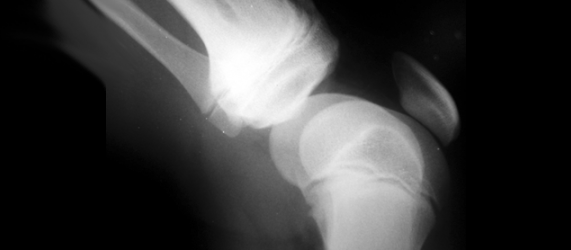
Tibial tuberosity issues typically fall under what is called Osgood Schlatter’s disease/syndrome. This occurs more in children because if they do a lot of physically exerting activity while their bones are elongating during puberty there is a potential for the bone to start pulling away away from the rest of the tibia.
As can be seen above this can be easily diagnosed by X-ray, and it will physically manifest as bumps on the shins that will be sore to the touch.
Treatment
Typical doctor recommended treatment is the RICE protocol. Activity should be limited to non-painful activities lest it be aggravated.
Like said in the above sections on tendonitis it is important to do soft tissue work to help loosen up the quads to exert less stress through to the tibial tuberosity. In this respect, foam rolling, massage, and light stretching should help significantly with the RICE protocol.
Posterior chain and proper biomechanics during running, squatting, lifting, etc. activities should also be examined to make sure that more stress is not being put on that area. However, generally this type of injury is more self limiting than the tendonitis issues.
Knee capsule / plica / medial collateral ligament / To the top


Photos from http://www.ortho.com.sg/ and http://www.floridaortho.com/
The tibial collateral ligament (MCL) is rarely injured unless there is an impact injury or severe fall or incident such that the leg is bent into an awkward position. It is one of the stronger knee ligaments since it is fairly big, so unless you have had one of these types of injuries I would say it probably is not one of these issues. Usually a MCL sprain accompanies other knee damage. If you suspect a problem with this ligament see a doctor.
The knee capsule and plica band can be easily aggravated given improper biomechanics or scar tissue around the area from surgery. This is why the pictures above are of plica and not the TCL/MCL because most type of pain here is likely not going to be of the ligament but rather the capsule and plica especially if there is a lot of cutting/torquing movements and bigger Q-angle.
Treatment
So if the injury is suspecting MCL see an orthopedic doctor.
Since the knee capsule and plica are more connective tissue typical modalities are aimed at reducing the aggravating inflammation. Thus, RICE, NSAIDs, and non-painful mobility and mobilization of the muscles around the area are generally prescribed. Also, other modalities to decrease inflammation such as iontophoresis or phonophoresis can be used, and as a last resort there is surgery.
Pes anserinus issues / To the top


Photos from http://www.jointventurespt.com/ and http://kneespecialistsurgeon.com
The pes anserinus (“goose foot”) is a group of tendons of the sartorius, gracilis, and semitendinosus muscles that insert medially and inferiorly (inside and below) to the knee joint.
To check to see if there is an issue with tendonitis or the pes anserine bursa this area can be palpated for pain, soreness, and sensitivity.
To check if it is the right area it should be approximately below the MCL and band of plica that sit directly medially along the knee joint. Additionally, if you are sitting and push your heel into the ground and feel for the semitendinosus tendon along the inside of the leg and follow it then it should and insert on the tibia in the position seen above.
Pes anserine tendonitis or bursitis can exist for a variety of reasons. From what I have seen it tends to occur there is improper biomechanical patterns and general overuse.
The most common pathologies I have seen this occur in is if there are the issue of collapsing knees (knees collapsing inwards) during movements such as squatting and running. Likewise, if there is hip internal rotation immobility or a foot pathology such as flat feet where the feet start to “toe out” or duck walk this may start to cause issues with the pes anserine (as well as many other pathologies in this article).
Treatment
Like the rest of the bursitis and tendonitis issues the typical treatment lies with RICE protocol, massage, and anti-inflammatories if necessary. Stretching, heat, and massage may be used on the muscles that make up the tendons to help loosen them up to take pressure off of the bursas and/or tendons to help improve healing.
If it is tendonitis we have an article On Tendonitis for how to deal with both acute and chronic tendonitis injuries.
Remember, if the injury is acute then the treatment(s) that are most effective are RICE protocol, mobility work, light stretching, massage to the muscle, and potentially anti-inflammatories.
If the injury is more chronic then a protocol that work best are mobility, stretching, heat, friction massage to the tendon, massage to loosen up the muscles, and eccentric exercise. Eccentric exercise is one of the only proven non-invasive methods for rehabilitation of chronic tendonitis. This is the most important factor of a chronic tendonitis regime. See the above tendonitis link for more on this.
Learning how to squat correctly by engaging the posterior chain (glutes, hamstrings, etc.) will help significantly take stress off of this type of injury. So that is definitely one of the things that can be focused on aside from other modality treatment. Exercise should be focused on sitting back on the heels and not coming up onto the toes because that puts more stress on the anterior chain.
Fibular head / biceps femoris / lateral collateral ligament / To the top

Photo from http://www.anytimehealth.com/
As seen above the biceps femoris as well as the lateral collateral ligament (LCL) both attack into the head of the fibula which is why I grouped them together.
Like the MCL, the LCL is often rarely injured without a significant impact or twisting injury so if you suspect as such you should see a doctor. If you are sitting you can check it’s integrity by sitting in cross leg position. Then feel underneath the knee for the bump that protrudes on the femur and the fibular head which should be below it. The ropey connective tissue that bridges between them is the LCL.
The fibular head should move in 3 planes when you flex and extend your ankle. If it does not move well then there may be an issue there if there is any type of pain in that area. When you dorsiflex the fibular head should move up, forward, and rotate outwards. The opposite should occur when you plantar flex.
To check the biceps femoris tendon you should put your knee at a 90 degree angle and locate the fibular head on the outside of the leg. If you dig your heel into the ground you should feel the biceps femoris tendon become taught and you can palpate if the area is painful, tender, or swollen.
In regards to the biceps femoris tendon like the pes anserine tendons it can also suffer from bursitis and tendonitis so if the issues are along that tendon as it runs into the fibular head then you probably know what it is.
Treatment
If the issue deals with the LCL or the fibular head not moving correctly then see an orthopedic doctor or physical therapist. Usually if the fibular head is not articular correctly it is a multijoint issue dealing with the foot, ankle, knee, and possibly the hip/SI joint/low back as well. When one thing gets gummed up so to speak other joints/connective tissues/muscles have to take up the slack. Thus, get it looked at by a professional.
If it is tendonitis we have an article On Tendonitis for how to deal with both acute and chronic tendonitis injuries.
Remember, if the injury is acute then the treatment(s) that are most effective are RICE protocol, mobility work, light stretching, massage to the muscle, and potentially anti-inflammatories.
If the injury is more chronic then a protocol that work best are mobility, stretching, heat, friction massage to the tendon, massage to loosen up the muscles, and eccentric exercise. Eccentric exercise is one of the only proven non-invasive methods for rehabilitation of chronic tendonitis. This is the most important factor of a chronic tendonitis regime. See the above tendonitis link for more on this.
Learning how to squat correctly by engaging the posterior chain (glutes, hamstrings, etc.) will help significantly take stress off of this type of injury. So that is definitely one of the things that can be focused on aside from other modality treatment. Exercise should be focused on sitting back on the heels and not coming up onto the toes because that puts more stress on the anterior chain.
Iliotibial band issues / To the top

Photo from http://www.itendonitis.com/
IT band (friction) syndrome is a multifactorial developmental process that leads to pain and inflammation in near the distal end of the IT band right near the knee joint. Since it is technically connective tissue that is inflammed and aggravated it can be treated like a typical case of tendonitis.
It’s etiology is very similar to that of patellofemoral syndrome where improper biomechanics, muscle imbalances, or anatomical issues can lead to its development. The various muscles that connect into the IT band do various things. The tensor facsiae latae assists in hip flexion, internal rotation, and abduction; the gluteus maximus is a prime mover of hip extension, abduction, and internal rotation.
Also, what is less known is that a majority of the vastus lateralis sits directly under the IT band itself as it extends fairly far up the lateral side of the leg. That means if the fascia between the IT band and vastus lateralis is tight for whatever reason being it overuse or immobility then that can also affect correct function of the IT band.
If these muscles get tight, overused, build up with scar tissue, etc. it can put a lot of tension on the rest of the IT band. In addition, the improper biomechanics like collapsing knees will also force a lot of stress onto the IT band because it is one of the only forces that prevents the knees from collapsing inwards besides the vastus lateralis and the LCL. Now you can see why patellofemoral syndrome (via vastus lateralis overdevelopment) is a similar issue to IT band issues especially with poor biomechanics.
Treatment
The treatment is very similar to the patellofemoral issues since connective tissue and articular cartilage have low blood supplies they need many things to help correct these issues.
First, bringing down the pain and inflammation is paramount. This can be done with the typical RICE protocol, massage, and anti-inflammatories if necessary.
Secondly, there must be loosening/strengthening of particular muscle groups. We want to strengthen the vastus medialis, vastus medialis obliquus, hamstrings, and glutes. We want to massage, trigger point, foam roll, tennis ball, etc. to loosen the vastus lateralis, rectus femoris, IT band, calves, hip flexors, etc.
Thirdly, we need to make sure there is enough range of motion at the ankles and hips. We want to especially gain more dorsiflexion in the ankles with calf stretches, and we would like to gain more hip extension by stretching the hip flexors as well as mobilizing hip internal and external rotation. In addition, in the case of IT band we need to stretch out the glutes and TFL.
Many of the specific stretching/strengthening exercises can be found here.
Lastly, we need to teach proper biomechanics by deemphasizing the anterior chain by sitting back more in squats, teaching proper running technique, etc.
In addition, the knees must NOT be allowed to collapse in during any exercise that is taught. This is paramount. One of the best ways to do this is to cue to spread the floor with the feet during squatting, lunging, etc. if the knees want to collapse inwards. If this is ineffective, a band can be placed to pull the knees inwards to force the the person to think about forcing the knees outwards during the movement.
Since the glutes are one of the potent external rotators of the hip they should be evaluated for weakness/inactivation especially if there is a lot of sitting during the day. Once you get them active not only will it help correct the technique, but it will make you significantly stronger as well.
ACL issues / To the top

Photo from http://www.youcanbefit.com/
I am only going to talk about ACL issues since PCL tears are quite a bit more rare.
First, if you suspect that you have an ACL tear you should see your orthopedic doctor to get tested. There are some tests that can be used such as Lachman’s, pivot shift, or anterior drawer tests, but these should be performed by a profession who knows what they are looking for.
Generally, if you have an ACL tear there will be some unmistakable symptoms:
1. Pain within the joint. Usually sharp from an impact or contact injury.
2. Many times a pop can be heard when the injury occurs
3. Usually the knee will swell fairly significantly
4. Instability when walking or running. The knee will feel like it will suddenly give out on you.
Directly after an injury it may be hard to confirm a diagnosis since if there is pain and swelling and general tightness of the muscles it may lead to some false positives.
However, diagnostic imaging is used in almost all circumstances to confirm before surgery is scheduled.
Finally, I must note that meniscus injuries sometimes present like ACL injuries and often happen concurrently with ACL injuries which means it is imperative that you seek proper medical attention instead of trying to self diagnose yourself. You will not be able to treat them yourself anyway which is why you should see an orthopedic doctor especially if your activities of daily life or athletic performance are hindered.
Treatment
If you have an ACL tear and want to get back to athletics you should get the surgery. Talk to your orthopedic surgeon and physical therapist.
You can live a perfectly normal life without an ACL as long as the surrounding musculature of the knee is strengthened properly. A repair is not needed in these cases. In some instances, athletes have been able to play on a torn or partially torn ACL for years without knowing they did drastic damage to their knee because they are strong and the muscles were able to stabilize the knee correctly.
If you have any questions about this type of injury talk to your physical therapist or doctor. Listen to your PT for rehabilitation options.
Meniscus issues (lateral and medial) / To the top

Photo from http://www.riversideonline.com
Meniscus injuries are an interesting topic. Like I stated in the ACL section they can sometimes present like ACL injuries and often happen concurrently with ACL injuries which means it is imperative that you seek proper medical attention instead of trying to self diagnose yourself. You will not be able to treat them yourself anyway which is why you should see an orthopedic doctor especially if your activities of daily life or athletic performance are hindered.
However, there are some similarities and a couple differences you can look for that may point towards a meniscus injury as opposed to an ACL.
1. Pain within the joint. Usually sharp from an impact or contact injury.
2. Many times a pop can be heard when the injury occurs
3. Usually the knee will swell fairly significantly. For a meniscus injury this may or may not occur.
4. Instability when walking or running. For a meniscus injury this may or may not occur.
Additionally, the meniscal injuries may also present:
5. Occasionally or often the knee will “lock” often when trying to straighten or bend the knee during any type of movement
6. The pain is usually localized towards one of the diagonal directions of the knee. The pain will be inside the joint but it will usually be localized towards the front or back and off to one side or the other. This is because the anterior and posterior horns of both meniscus are the easiest to damage during an impact and/or with a twisting action that messes with the proper articulation of the bone.
If you suspect a meniscus injury please see your orthopedic doctor to get a confirmation and your options depending on the extent of the injury.
Treatment
There are a fairly large amount of different types of meniscus tears and a significant degree in the extent of injuries. Sometimes they can be repaired; sometimes the menisci will have to be removed.

Photo from http://www.foundrysportsmedicine.com/
There are some instances where you may not need arthroscopic surgery and the meniscus can heal itself although they are more rare. Injuries in the “white zone” tend to have no vascularization which means the body cannot repair the injury itself. However, if the injury is in the “red zone” that means the body has some limited degree of blood supply there where it may possibly heal the injury (depending on the extent of the damage).
However, even if the injury is in the red zone if the tear breaks through the rim of the meniscus that may cause significant destabilization of the knee so there may be problems with non-surgical options even if the tear can heal itself.
Again, your best bet is to see an orthopedic doctor and get assessed. They will likely do some tests such as McMurray’s and Appley’s compression test as well as confirm it with medical imaging such as MRI like they would with an ACL.
If you have any questions about this type of injury talk to your physical therapist or doctor. Listen to your PT for rehabilitation options.
Muscle strains / To the top
Strained and pulled muscles will tend to be in the muscle belly of the tissues which means that it will hurt right inside the muscles. Strains typically occur during lifting or activities where the body is put under a lot of stress especially when fatigued.
If the pain is located in the quadriceps or hamstrings themselves they it is likely you have some form of strain or at least tight muscles/scar tissue/adhesions in the muscle(s).
In the case of muscles strains or pulls unless it is extremely bad where your tissues are turning black and blue and you absolutely need pain killers, you probably do not need to a see a doctor. This is because you will most likely just get a prescription for pain killers and be told to rest.
However, if you are that worried about your injury then do not hesitate to see a doctor or physical therapist. Better safe than sorry.
Treatment
I have already written extensively on muscle strains which will help you get started on the road to recovery.
The back of the knee / To the top


Photos from http://www.fpnotebook.com and http://www.5skaggs.com
In almost all cases, especially if there is some type of bruising any back of the knee injuries will likely be some type of muscle strains.
As you can see from the above image there is mostly only ligaments crisscrossing the knee joint, and then muscles running around doing various actions on the knee. The plantaris tends to be inconsequential but the hamstrings, popliteus, and both heads of the gastrocnemius all play multiple roles in the proper function of the knee joint.
Hyperextension injuries are the most common cause of pain on the back of the knee, and if they are severe enough the injury is likely to be the ACL which helps to prevent anterior translation of the tibia on the femur.
Thus, the other most common type of injury is strains of the aforementioned muscles. But if you have any doubts about the diagnosis, see a doctor or physical therapist.
Treatment
If you suspect ligamental damage, again see an orthopedic doctor or physical therapist.
If you suspect a strain I have already written extensively on muscle strains which will help you get started on the road to recovery.
Other pathologies / To the top
There are multiple other pathologies which can be present with knee injuries. For example, nervous system and radicular issues, fractures, cysts, cancer, etc.
Obviously, for everything I have not covered it is important to get checked out by a qualified professional.
Treatment
Other problem(s) may show up even if you have a diagnosed pathology, so it is important to be under the plan of care of a orthopedic doctor or physical therapist who you can trust to talk about your injuries and any concerns you have about your rehabilitation.
Remember, there are good and bad doctors and good and bad physical therapists. If you don’t have a good one who can answer your questions and provide you with a good rehabilitation program or options then you can always find another.
If you are an athlete specifically you may want to look for doctors and physical therapists who work with sports teams.
I hope this article was helpful in determining any potential knee injuries and what some of the options are about treating such dysfunctions.
Remember however that this is the Internet and even though this article may be right 90% of the time in correctly figuring out a pathology it should not be used as a definitive guide for injury diagnosis and treatment.
You should always talk to your orthopedic doctor or physical therapist for a confirmation on diagnosis and treatment especially if you have any questions regarding a certain pathology and subsequent rehabilitation process.
If you suspect you have an injury that does not fall into any of the categories above see a medical professional immediately. Also, if you have an injury which presents debilitating pain or presents possible insidious neurological symptoms such as sensory or motor deficits see a medical professional immediately. Motor deficits are critical enough that you may want to go to the ER ASAP.
Disclaimer: Any information contained herein is not professional medical or physical therapy advice. Always consult your doctor or physical therapist before using such information. For more details see our full site terms and conditions.
Author: Steven Low
Steven Low is the author of Overcoming Gravity: A Systematic Approach to Gymnastics and Bodyweight Strength (Second Edition), Overcoming Poor Posture, Overcoming Tendonitis, and Overcoming Gravity Advanced Programming. He is a former gymnast who has performed with and coached the exhibitional gymnastics troupe, Gymkana. Steven has a Bachelor of Science in Biochemistry from the University of Maryland College Park, and his Doctorate of Physical Therapy from the University of Maryland Baltimore. Steven is a Senior trainer for Dragon Door’s Progressive Calisthenics Certification (PCC). He has also spent thousands of hours independently researching the scientific foundations of health, fitness and nutrition and is able to provide many insights into practical care for injuries. His training is varied and intense with a focus on gymnastics, parkour, rock climbing, and sprinting. Digital copies of the books are available in the store.