This post is an analysis of common orthopedic problems that arise from shoes and sitting, how to evaluate their development, and finally a look at how to implement prehabilitation or rehabilitative protocol to improve their condition.
Table of Contents
- Introduction
- Shoes
- Sitting
- Systemic biomechanical issues
- Evaluation of lower body dysfunction and correction
- Soft tissue optimization and corrections
- Conclusion
Read time: 45-60 minutes.
1. Introduction
Note: We have an in-depth article on the feet as well, however, it does refer back to this article so I would suggest reading both if you have foot issues.
Shoes and sitting. Two things that are ubiquitous in modern society.
There has been media sensationalization of the detrimental effects of shoes. However, there has not been a lot on sitting other than upper body alignment issues. Do these two things really have that much of an impact on our lives? Or is it just athletes?
Unfortunately, most information out right now does not look specifically at the effects that injuries have on the body as a system. Rather, most of the solutions to problems tend to focus on only reducing the pain or alleviating the problem at one joint specifically. For example, shoulder strain can manifest in rotator cuff problems, but that strain may be from a cascade of other issues such as loss of thoracic extension, loss of proper scapular movement, and incorrect muscular activation.
More recent studies such as this 2015 show that Going barefoot: Strong ‘foot core’ could prevent plantar fasciitis, shin splints, and other common injuries.
2. Shoes
There have been numerous articles in the past saying how shoes are bad for you. For example,
- You Walk Wrong,
- The painful truth about trainers: Are running shoes a waste of money?,
- Footwear Alters Normal Form And Function Of The Foot
- Barefoot running debate – GREAT image that shows some of the dysfunctions we will look at later.
- Barefoot Running: How Humans Ran Comfortably and Safely Before the Invention of Shoes
In general, these are true. For example, this abstract published in the Journal of the Southern Orthopaedic Association in 1994 states:
The shod foot and its implications for American women.
Throughout history, members of human societies have gone barefoot, and those societies seemingly had a low incidence of foot deformities and pain. Only one study has addressed the problem of infection through injury to the bare foot; otherwise, the unshod foot seems to have had minimal problems. Initially shoes were made in the shape of the foot and were sandals. Over time, shoes became decorative items and symbols of status and vanity. As the shape of shoes changed, they became deforming forces on the foot and the source of pain. Recent studies by the Council on Women’s Footwear of the American Orthopaedic Foot and Ankle Society have tried to document the problems caused by shoes on the feet of American women. Attempts should continue to educate women on appropriate shoes and proper fit.
These are not the only cases. Another instance is this abstract from the August 1991 issue of Pediatrics.
Shoes for children: a review.
1. Optimum foot development occurs in the barefoot environment. 2. The primary role of shoes is to protect the foot from injury and infection. 3. Stiff and compressive footwear may cause deformity, weakness, and loss of mobility. 4. The term “corrective shoes” is a misnomer. 5. Shock absorption, load distribution, and elevation are valid indications for shoe modifications. 6. Shoe selection for children should be based on the barefoot model. 7. Physicians should avoid and discourage the commercialization and “media”-ization of footwear. Merchandising of the “corrective shoe” is harmful to the child, expensive for the family, and a discredit to the medical profession.
These are some pretty harsh words. However, beyond that let’s dig a little deeper by looking at shoes and running.
The incidence of running injuries before the 1950s was low. But since the 1970s when shoe manufacturers have started to put more and more padding into shoes, the incidence of runners that have some injury every year is up to nearly 60%. Some of the cause could be to due confounding factors such as the rise in obesity, improperly fitted shoes, and so on. However, there is at least some reason to believe otherwise.
Most of the common running shoes have lots of padding in the heel which incorrectly gives the user an impression that heel-toe running is correct. Significant amounts of heel-toe running can potentially cause long term damage in combination with other factors such as obesity, improperly fitted shoes, and strenuous activity, especially in children and the elderly. In heel-toe running, the joints are taking the impacts rather than your musculature dissipating the force correctly with mid- and fore-foot striking. One study showed that shoes mechanically alter stride compared to barefoot running resulting in lower net efficiency.
It is also important to understand that walking, in which the heel strikes the ground first, is a fundamentally different gait from jogging, running, and sprinting which require a mid- and fore-strike to protect the body and operate at a high level. Walking does not have the high-repetition high-impact movements that the other gait motions have, which means it is not going to be potentially injurious for the body.
However, beyond the walking and running mechanics, let us analyze why shoes are a problem.
- Most shoes now have an elevated heel as padding. In walking or running, the knee tracks over the toe as you take a step. With an elevated heel, the foot is already tilted forward which means the ankle does not need to bend as much during movement. Not taking a muscle often to the edge of its range of motion means that the muscles start tightening up. This limits the range of motion (ROM). Thus, with shoes there tends to be a loss of 10-20 degrees range of motion in ankle leading to tight calves.
- The padding in the shoes is problematic as well. Our body and feet have proprioceptors that allow us to feel the ground as we are moving. This gives us the ability to make small corrections to maintain proper posture and movement. The padding in the shoes allows improper corrections to be made (as they will not be punished by awkward landings), and decreases our natural proprioceptive ability and affect ankle coordination abilities. This leads to inactivated muscles on the plantar aspect (bottom) of the foot and decreased ankle stability especially with inversion and eversion corrections. In addition, this may lead to increased frequency of falls in the elderly.
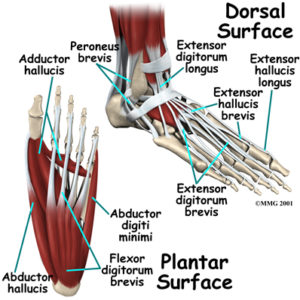
As you can see, shoes are a problem especially compared to barefoot ability. This is even more evident if we are aware of the fact that the plantar aspect of the foot has 3 different muscle layers including the plantar fascia. Let’s now take a look at some more studies supporting the two points above.
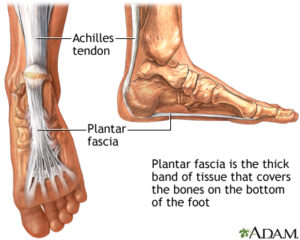
Photos from medlineplus and eorthopod
This study showed that “a significant increase in leg stiffness from the barefoot to the “cushioned” shoe condition was noted during hopping. When running shod, runners landed more dorsiflexed (foot tilted upward) but had less ankle motion than when running barefoot. […] The primary kinematic difference was identified as running speed increased: runners landed in more knee flexion. At the ankle, barefoot runners increased ankle motion to a significantly greater extent than did shod runners as speed increased.” When running barefoot, the forefoot receives the ground** with less than 90 degrees of dorsiflexion. The decreased range of motion is important to note.
** Minimalist shoes like sprinters use with proper technique show similar biomechanical patterns as barefoot running.
Likewise, flatter foot touchdown and increased leg stiffness was found in barefoot running. Increased “leg stiffness” is good because that means the muscles are taking the brunt of the forces rather than your joints.
One study on ankle sprains showed that awareness of foot position is impaired by shoes. The authors also noted that there was increased muscle activity during inversion with shoes. They concluded that this was the body’s adaptive mechanism to oppose the increased tendency to roll the ankles with shoes as opposed to barefoot.
In a similar vein, this investigation showed that as the “shock ability” of the materials in running shoes decreased, foot control (proprioception) increased. Loss of proprioception is implicated in as much as 50% of running shoe injuries!
“This experiment showed that the sandals not only restricted the natural motion of the barefoot but also appeared to impose a specific foot motion pattern on individuals during the push-off phase.”
The best evidence, however, as far as we are concerned it from actual biomechanical evidence. This can be seen clearly in this study of the biomechanics of shod vs. barefoot running.
Results
Increased joint torques at the hip, knee, and ankle were observed with running shoes compared with running barefoot. Disproportionately large increases were observed in the hip internal rotation torque and in the knee flexion and knee varus torques. An average 54% increase in the hip internal rotation torque, a 36% increase in knee flexion torque, and a 38% increase in knee varus torque were measured when running in running shoes compared with barefoot.
We will talk extensively about internal rotation, valgus, and varus states. The discussion here provides an ample preview:
The observed 36% increase in the knee flexion torque with running shoes potentially increases the work of the quadriceps muscle, increases strain through the patella tendon, and increases pressure across the patellofemoral joint. Furthermore, a 38% increase in the knee varus torque implies relatively greater compressive loading on the medial tibiofemoral compartment, an anatomical site prone to degenerative joint changes, as compared with the lateral compartment. Finally, the disproportionately large 54% increase in the hip internal rotation torque may have particularly high clinical relevance, given previous findings that indicate that competitive running may increase the risk of OA of the hip joint.
The internal rotation torque and quad dominance in particular in conjunction with tight calves are some of the main reasons of the dysfunctions we will discuss later.
Finally, we have this study which indicates that “selecting shoes based on plantar shape had little influence on injury risk.” Basically, no matter how expensive your shoes or how much ‘support’ they provide, they don’t decrease your injury risk. This is a very strong case for flats/minimalist shoes/barefoot. This article on the ankles also provides some relevant material to the discussion.
Note: The loss in range of motion from the calves covers why I do not have to mention why high heels are terrible for women. Even though women look good in them. Similarly, in sports with extensive plantar flexion such as pointing the toes in gymnastics and figure skating it is possible to develop similar problems.
3. Sitting
Sitting has become a huge problem in modern society. Sitting is obviously common for school and most jobs. However, throw in decreasing amounts of recess and lack of activity for adults as well as obesity and you have a full blown epidemic.
There has not been much talk of this in the media. However, most of the sports communities knows the problems associated with sitting and its detrimental effects on athletic performance. Even so, the effects of sitting are more widespread than just poor athletic ability. Let us analyze why sitting is a problem.
- In sitting, the butt / gluteal muscles are in a stretched position. When a muscle is allowed to be in a stretched position for extended periods of time such as in school or office jobs, the muscle tends to become weaker and inactivated. This is the opposite of what happens with the calves in their shorter and tighter position. Thus, with sitting the glutes become weak and inactive.
- The hip flexors which are shortened in hip flexion, like the calves, become shorter and tighter. The hip flexors consist of the iliopsoas, rectus femoris, sartorius, tensor fasciae latae (TFL), and adductors longus and brevis. Thus, with sitting the the hip flexors become short and tight.
Photos from blogpost and chiropractic-help
It has been investigated “whether gluteal muscles could be activated more effectively by stimulating the proprioceptive mechanism during walking.” They came to the conclusion that balance shoes help especially with lower back pain helping fire inactivate gluteal muscles. Ironically, you could just walk barefoot and do balance work to stimulate foot proprioceptors as well as do gluteal activation work. We will get to this later.
There are varying degrees of inactivation. Gluteal inactivation does not mean that the glutes fail to contract altogether. Rather they will fire although with decreased intensity and/or a delayed pattern which may be ineffective during proper recruitment during certain movements.
There is another interesting study done on a variety of subjects.
RESULTS: There were 1832 deaths (759 of cardiovascular disease (CVD) and 547 of cancer) during 204,732 person-yr of follow-up. After adjustment for potential confounders, there was a progressively higher risk of mortality across higher levels of sitting time from all causes (hazard ratios (HR): 1.00, 1.00, 1.11, 1.36, 1.54; P for trend <0.0001) and CVD (HR:1.00, 1.01, 1.22, 1.47, 1.54; P for trend <0.0001) but not cancer. Similar results were obtained when stratified by sex, age, smoking status, and body mass index. Age-adjusted all-cause mortality rates per 10,000 person-yr of follow-up were 87, 86, 105, 130, and 161 (P for trend <0.0001) in physically inactive participants and 75, 69, 76, 98, 105 (P for trend = 0.008) in active participants across sitting time categories. CONCLUSIONS: These data demonstrate a dose-response association between sitting time and mortality from all causes and CVD, independent of leisure time physical activity. In addition to the promotion of moderate-to-vigorous physical activity and a healthy weight, physicians should discourage sitting for extended periods.
The very intriguing thing to note here is that sitting, even when adjusting for smoking, physical activity, and other mortality factors, has a dose-response association (meaning that the more you sit) the higher your risk of death. The P-value for this is <.00001 which means the data is particularly strong: 99.999% of the time this data set would not occur randomly. Sitting is insidious and dangerous the more you do it.
Another study seems to verify this conclusion. After adjusting for physical activity and other factors, those who sat greater than 6 hours per day were 37% more likely to die than those who sat less than 3. With a lack of physical exercise those who sat greater than 6 and less than 3 hours were 94% and 48% respectively more likely to die. Associations were strongest for cardiovascular disease mortality.
Consider that we now all send our kids to school for 7-8+ hours a day for 15+ years, and have desk jobs for much of our adult lives…. this is not a good sign.
Note: there will be more studies to come on gluteal activation; however, as a lot of them relate to the injuries that is specifically why they will be discussed later. I just want you to know that I do have my position on this topic supported at least as much as I have supported my case against shoes.
Shoes and Sitting Conclusion
In conclusion, we learned that shoes and sitting cause many problems. This is a big problem because they are ubiquitous in modern society. Shoes tend to allow the user to run improperly (heel-toe) and hinder proper ankle biomechanics. In addition,
Shoes tends to cause the problems of
- Tight calves resulting in loss of 10-20 degrees of dorsi-flexion ROM in the calves.
- Inactivation of the muscles on the bottom of the foot and the ankle stabilizers.
- Decreased proprioception of the lower limbs.
Sitting tends to cause the problems of
- Inactivation of the gluteal muscles.
- Tight hip flexors (i.e. iliopsoas, rectus femoris, sartorius, tensor fasciae latae [TFL], and adductors longus and brevis).
In the next segment we will discuss look at the systemic biomechanical issues that arise from these deficits. Click below for the next part.
4. Systemic Biomechanical Issues
Here is what we learned in the previous section. These points will be the key to elucidating how movement dysfunction develops.
Shoes tend to cause the problems of
- Tight calves resulting in loss of 10-20 degrees of dorsi-flexion ROM in the calves.
- Inactivation of the muscles on the bottom of the foot and the ankle stabilizers
- Decreased proprioception of the lower limb
Sitting tends to cause the problems of
- Inactivation of the gluteal muscles.
- Tight hip flexors (iliopsoas, rectus femoris, sartorius, tensor fasciae latae [TFL], and adductors longus and brevis).
There are two different ways the body will compensate because of these problems. The first is having the shins angle inward (the knees come toward each other). This is called valgus stress. The second is having the shins angle outwards away. This is called varus stress. In regards to sitting and shoes, valgus stress tends to be more common for multiple reasons, so I will be discussing that most of the time. I will only talk about varus stress briefly. Those that are interested in further reading may contact me later.
Valgus Stress
Valgus stress is more common because it is a compensation from multiple aspects of shoes and sitting that we have described before. The body naturally compensates when it cannot perform its abilities. For example, if you smash your leg against a corner you naturally compensate with a limp to avoid putting pressure on the injured limb until the pain subsides. Similarly, if your shoulder is hurting you will naturally compensate by side bending in your spine to get your arm overhead.
It is common for the body to naturally compensate with valgus stress because of shoes and sitting. The first “symptom” that usually appears for most people is inward tracking knees. This occurs for multiple reasons.
- First, the loss in 10-20 degrees of ROM from the calves must go somewhere. The next joint above the ankle where the ROM is lost is the knee. Thus, range of motion may be gained by rotating the knee inward.
- The glutes, especially gluteus maximus and medius, are potent external rotators of the femur. Since the glutes are inactivated with sitting, the femur is allowed to rotate internally in knee bending. This lack activation allows the knees to deviate inward too.
- Adductor longus and brevis are tight and shorter from sitting. The gluteal muscles are also abductors of the femur. Since the glutes are inactivated from sitting, the adductors will tend to pull the knee inward as it bends (eccentric movement).
- Adductor magnus is involved in hip extension. Since the glutes which are primary hip extensors are inactive, a strong OR weak adductor magnus will tend to pull the knee inward as it straightens (concentric movement).
Note: The adductor issues are two separate issues and should not be grouped together. The biomechanical issues with both will have some differences when we discuss how to correct the issues later.
Note 2: It seems there is some confusion on the theory of weak adductors and valgus (Starting Strength pg 46-49). The weakness in adductors is specifically for adductor magnus which lets the knees cave in during the concentric. As I said, this is a separate issue from the knees caving in on the eccentric. What happens with a weak adductor magnus is that coming up from the bottom of the squat the hip extensors are at their longest position. Muscles are normally strongest at the middle of their range of motion shown on the force-length curve. This means that the knees cave in to shorten the magnus towards the middle of its range of motion where it is the stronger. If the glutes and abductors were active and stronger this would not happen; however, since they are more inactivated, the adductor magnus along with the hamstrings become primary hip extensors thus pulling the femur medially.
Why is the lost ROM in the calves such a big issue? Well, this study in tennis players shows that restricting ROM in the ankle “may also provoke large internal forces elsewhere.” Stiff shoes were found to the be the worst, and ones that moved better were superior. Obviously, the natural foot itself would be the most flexible in regard, but unfortunately cannot be used by itself extensively on extremely rough surfaces.
Inward tracking knees tends to precipitate a cascade of alignment and biomechanical dysfunctions which affect the other muscles, connective tissue, and eventually the joints within the legs.
Muscle and connective tissue issues
- Flat feet / pes planus / collapsed arches – Internal rotation torque and medial tibial tilt at the talus put most of the weight distribution on the medial arch of the foot. Combine this with inactivated muscles on the plantar foot from the shoes, and the arch collapses. The picture shown below compares a foot with a correct arch (top) to that of a fallen arch (bottom)

Photo from podiatrytoday.com
You can test this by standing up and allowing the knee to track in. You will see and feel that the tibial torsion at the talus pronates the foot and allows the majority of the weight to rest over the medial arch of the foot.
This analysis of increased forefoot loading (from higher heel shoes) leads to greater medial stress on the foot as well. Likewise, this study showed that there is greater stiffness in the forefoot especially during barefoot running compared to running with shoes. This is good in the respect that the plantar aspect muscles are firing to maintain the arch. A lack of stiffness in the foot indicates that the muscles are not firing effectively and thus a greater flattening of the arch is occurring in strides. Repetitive stress like this may lead to collapsed arches.
- Plantar fasciitis – Like flat feet the inactive muscles on the foot allow the arch to collapse some putting stress on the plantar fascia. Tight calves contribute as the fascia from the plantar foot is continuous up the posterior chain and pulls on the calcaneus.
It is likely that you only develop either flat feet or plantar fasciitis. Although it is possible to develop both. If your plantar fascia is more lax and stretches easier, it is easier to have the arch collapse all the way even before plantar fasciitis may develop. When the intrinsic muscles of the foot are inactive, the plantar fascia is the last stopgap that holds the medial arch together before it collapses. Since the connective tissue is not built to take that kind of stress, it gets inflammed and painful.
Extremely tight calves, and extended time with heel elevated shoes may lead to this condition solely. A lot of it is variable depending on the person. Remember, I am just describing some of the cases.
- Achilles tendonitis and rupture – the internal rotation torque and medial tilt of the tibia at the talotibial joint in combination with plantar flexion in movement increases the likelyhood of damaging the achilles. All tendons and ligaments work best when pulled on directly like a piece of paper, but when you twist a piece of paper and pull it tears more easily.
In respect with past runners the incidence of achilles injuries has decreased. This is because the calves were involved more when footwear was minimal. But now, with decreased ROM in the calves, the injuries tend to migrate elsewhere. We will see this in the following points.
The torque at the ankle and thus achilles tendon especially in movements on the toes makes this injury appear more frequently than it should. This is in combination with very tight calves.
- ACL sprains and tears – like the achilles the inward tracking knee tends to torque the ACL. Thus, spraining and tearing the ACL is more likely.
Note the inward tracking does also stress the MCL. But for time purposes I am not including this. Just know that in the event of a torn ACL with twisting there is often accompanying MCL sprain or tearing as well. In severely traumatic injuries the unhappy triad (ACL + MCL + meniscus tear) often occurs.
Photo from kcchampionperformance.com
At this point we need to note that women have increased incidence of ACL injury especially because of Q-angle. Womens’ hips are wider for child birthing and thus their knees have to travel further in at an angle under them to support their weight. This greater angle obviously leads to increased torque on the connective tissues at the knee.
This analysis demonstrated that valgus knee angle puts more stress on the ACL as their experiment showed that women land more often in knee valgus position. However, they found no different in gluteus medius activation between the sexes. I do not find the difference in gluteus medius activation troubling since both men and women are both sitting for 7-8+ hours a day in the classroom and doing homework. It would be an interesting comparison if they compared athletically dominant men and women versus the rest of the population though.
- Quadriceps dominance and tightness – the body senses the stress on the ACL from its proprioceptors. If the knees cave in too much obviously it is going to stretch out the ligaments or tear them. To stop this it strongly strengthens the quadriceps, especially the lateral aspect of the quad.
Women as well as men both develop this problem because everyone has a Q-angle. In addition, because the glutes are inactivated, the decreased force output of the hip extensors is compensated by the quads which are the knee extensors. This is also why women tend to be less athletically inclined than men, and also why quad dominant men are not-so-good athletically. For example, this study shows higher vastus lateralis development, higher quad to hamstring strength ratio, and lower gluteal activation in women because of Q-angle and valgus knee stress. This quad dominance in women is indicative of a higher risk of ACL injury than men. Similar results were obtained in this study examining Q:H imbalance in both the medial and lateral aspects of both the quads and hamstrings.
This study showed that increasing heel height (especially with high heels) increases quadriceps activation. There were no intensity increases but with muted glute function we do not need increases in repetitive intensity to see quadriceps dominance to develop. After all what we practice we get better at. If we practice “activating” the quads, we will develop quad dominance. This will also be a key later in redeveloping gluteal activation and strength.
Quad dominance does not only have to do with ACL injuries. Increased quad eccentric loading has been shown to be implicated in the development of patellar tendonopathy/tendonitis.
- Tensor fasciae latae (TFL) and iliotibial band (IT Band) tightness – since the glutes (especially gluteus medius) are weak, the TFL compensates for the body to maintain proper abduction abilities. In addition, increased stress is placed on the TFL and IT band when the knees cave in which strengthens these structures.
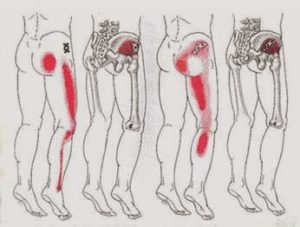
Pain referral pattern of TFL — Photo from newhealthadvisor.com
TFL and IT Band tightness, in combination with lateral aspect quad dominance often lead to patellofemoral syndrome where the patella starts tracking off to the lateral side of the knee. In addition, this may cause chondromalacia patellae which is wearing down the articular cartilage on the underside of the patella causing pain. An extremely tight TFL and IT Band also may cause IT band syndrome as well. In IT band syndrome, the IT band and TFL get extremely tight and start rubbing against the femur itself or other muscles in the area. This creates pain and inflammation.
Increasing the strength of the glutes to take forces away from the knee and back properly to the hip, like this one case study with gluteus maximus and medius strengthening showing improvements in patellofemoral pain. The same is true in this study of iliotibial band syndrome. There are even cases where a tight IT band and TFL with a weak gluteus medius can contribute to lower back pain.
- Hamstring weakness and tightness – as we have discussed, the quads become extremely strong and tight, this anteriorly translates the tibia with respect to the femur. This also puts stress on the ACL. To protect joint integrity (anterior-posterior) the body will lock down the hamstrings into extreme tightness to protect the ACL from sprain and rupture.
All quad dominant men have extremely tight hamstrings which are often extremely weak. Women, who tend to have less muscle mass overall, also have their hamstrings lock down. However, since there is less mass to protect the joint it also increases the likelihood of ACL rupture. We’ve been talking about it before but increased Q-angle, quad dominance, and this all contribute to the 3:1 ratio of women:men in ACL tears.
Athletically inclined quad dominant males and females will often have tight strong hamstrings. This is the other alternative, so it does not necessarily mean hamstring weakness is universal. Since the glutes are inactivated, the hamstring takes over the hip extension and will thus be stronger. Tight, strong hamstrings are notoriously difficult to loosen up. However, tight hamstrings are often prone to hamstring and groin strains/pulls as well. Incidentally, the decreased activation of the glutes increases the propensity of hamstring overloading and strain. Hamstring tightness may also be instigated or exacerbated from sitting in slouched positions for longer periods of time.
- Deep intrinsic butt muscles tightness – as we know the gluteal muscles are inactivated, so the deep intrinsic muscles lock down to protect hip joint integrity.
Normally this is not as important as the other dysfunctions, but some conditions can arise from this such as piriformis syndrome, SI joint, and lower back pain. In some of the population the sciatic nerve runs through the piriformis muscle in the buttocks. Thus, when the piriformis becomes tight and locked down because of gluteal weaknesses you will often see pain in the glute area and often radiating on down into the leg.
Gluteal weakness (2) and problematic activation patterns (2), (3), (4). Similar findings are true with SI joint pain (2). Now what causes gluteal weakness and incorrect activation patterns? Yes, sitting.
Also, as we stated before decreased hip ROM / mobility refers the mobility to another joint. The next joints in line are the SI joint and lower back. The SI joints and lower back are not meant to be mobile. When you increase the range of motion in those joints you often see increased incidence of sharp pain in the SI joint, potential for bulging and herniated discs, and asymptomatic lower back pain.
Joint issues. I put these last because usually it takes months or years within the aforementioned muscle and connective tissue imbalances to develop joint issues. Our bones remodel to the stress we put on them, and bone tissue is turned over every ~3 months or so. If our posture and biomechanics are out of alignment it will stress the bones and will eventually result in deformity.
In the case of valgus stress, most of the joint deformities are listed in this wikipedia article on valgus deformity.
- hallux valgus – or bunions are formed by repetitive inward tracking stress and weight distrbution over the medial arch.
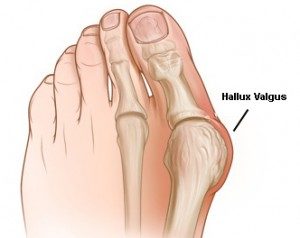
Photo from shopclues.net
There are actually two cases of how this occurs.
Repetitive stress over the medial arch plus the talar medial tilt will start to collapse the arch. Since all of the bones of the foot are connected, the stress from the collapse must go somewhere. The stress does not deform at the ankle where the bones and ligaments are the stronger. Rather the stress translates out to the farther part of the arch which is at the 1st metatarsal-phalangeal joint. Since the foot is on the ground and has the 2nd metatarsal next to it, hallux valgus forms by pushing the head of the 1st metatarsal outward. This is the place of least resistance (rather than upwards). Thus, most of these types of bunions are associated with collapsing arches / flat feet.
Alternatively, in some cases the inward stress at the knees pushes the ankle into varus (or higher arches). A varus ankle will twist the proximal metatarsals laterally and superiorly. This makes the head of the 1st metatarsal deviate medially and inferiorly. Obviously, since it cannot deviate inferiorly, it only deviates medially forming the bunion.
- Collapsed arches – the intrinsic muscles of the foot are inactive plus more medial weight lead to the collapse.
We already discussed this before, but permanent collapse is possible if allowed to last too long. The bones of the foot will adopt a more permanent planar foot configuration, often with bunion formation. Collapsed arches is one of the other ways valgus stress can be initiated. For example, collapsed arches tilt the talus. This makes the foot pronate. The pronated foot ‘encourages’ the tibia to internally rotated and tilt medially as well. You may see valgus stress appear in people with severely pronated feet even if their upper leg and patella are still oriented forward compared to the foot pointing outward.
Other deformities that may occur, but aren’t really much of an issue for those of you reading this.
- talipes valgus – inward tracking knees and talar medial tilt results in the ankle joint being deformed to the stress.
- genu valgum / knock knees – the medially and internal rotation tilt of the tibia and femur may lead to this.
- coxa valga – this deformity is actually not that noticeable by the layperson. Fortunately, it does not really need to be that noticeable because it is mainly only seen in children.
One of the reasons why soccer is the sport with one of the highest incidences of injury is because of extreme amounts of repetitive use combined with improper strength and conditioning. For example, this study on soccer shows that it exacerbates the valgus related stresses because most of the weight is distributed medially in soccer movements.
Valgus stress and pronation has been indicated in weight distribution over a smaller area of the foot. This is an increased weight to surface area ratio which means that it is more likely to develop injuries with the valgus condition compared to the varus. Another reason why valgus injuries are more common.
Also, remember that my descriptions are only one way to develop such injuries. Some people with flat feet just have decreased proprioception from shoes and that is enough to allow their arch to collapse. That then tilts the talus and the knee tracks inward from there. So there are definitely many cases for how different injuries arise.
The one thing we must keep in mind is that the body functions as a unit and usually it goes until it breaks in one area. Thus, we generally only have the propensity for developing one such injury at a time. On the other hand, it is certainly possible to develop multiple injuries depending on the person. In most people I have seen with at least one of the injuries described above, they have at least 2-4 if not more of the symptoms of valgus stress on their lower body. Keep this is mind later when you are analyzing yourself.
Varus Stress
I am only going to be briefly talking about this because for one it is not very common to have issues relating to this stress deformity.
The other way that the loss of range of motion in the calves is compensated for is with external rotation of the hip. This may result in varus stress especially if the knees come outward. However, this is rare. External rotation of the hip is most common in the elderly. As we sleep all of our muscles relax. If you sleep on your back (which is how you should sleep), most people allow their legs to relax with the feet pointed out. When you are in this position for 8 hours, much like sitting this allows the external rotators of the hip to become tight and the internal rotators to be stretched out and weak. Thus, hip, knee, foot turned out posture is developed from both sleeping, and loss of range of motion the calves.
The “most” common symptoms are at the feet and ankles again because of increased weight distribution on the lateral aspect of the foot. Fortunately, the associated conditions are high arches and the increased propensity to roll the ankles. This is in comparison to development of hallux equinovarus / club foot which is more common in children with developmental problems.
Suffice to say for most people with high arches or chronic ankle rolling it is important to avoid shoes especially with padding because they encourage this nonsense. We will talk about this later as well.
Conclusion
In conclusion, we learned that the valgus stress of inwards tracking knees is propagated by shoes and sitting because
- The lost ROM from the ankles is gained at the next joint which is the knees.
- Inactivated glutes which are external rotators allow the femur to rotated internally which encourages inwards knee tracking.
- The tight adductor longus and brevis in conjunction with the inactive glutes pull the knee medially in eccentric movement.
- Adductor magnus in conjunction with in inactive glutes pull the knee medially in concentric movement.
These can lead towards the muscle, connective tissue, and joint issues of
- flat feet / collapsed arches / pes planus
- plantar fasciitis
- achilles tendonitis or rupture
- ACL sprain or rupture
- quadriceps dominance and tightness
- tensor fasciae latae dominance and tightness
- iliotibial band tightness
- hamstring tightness (weakness or strength)
- deep butt muscle tightness
- SI joint or lumbar back pain
- hallux valgus / bunions
- talipes valgus
- genu valgum / knock knees
- coxa valga, while possible, is usually a developmental issue
After having reread the Neanderthal No More Part one article, Cressey and Robertson have come to a lot of the same conclusions I did (before me of course). It’s worth a read for their take on the same thing as well.
In the next segment, we will talk about how to evaluate dysfunctions and some corrections you can make.
5. Evaluation of lower body dysfunctions and corrections
Now that I have taken you extensively through common muscle, connective tissue, and joint problems associated with shoes and sitting we are going to discuss the ways to fix these dysfunctions.
Unfortunately, I do not have room to discuss all of these conditions that in depth because whole chapters in books are writing on single conditions that I have described. However, I will try to provide a basis with which you can systematically evaluate your own body to ensure that you have your muscles, alignment, and biomechanics in the normal ranges. This will ensure a very low probability of developing such injury conditions or for fixing the ones you have.
There are three main ways that you can evaluate potential problem areas. These are muscular, alignment and movement analysis. I am going to talk a bit about each. You should know, however, that as much as I can give details about descriptions for how to do this, it only comes through experience. Just like you have to coach many people to be able to correctly refine your technique of evaluating movement, you also have to be able to look at someone closely and be able to examine muscular, postural, and movement deficiencies.
Physical therapists tend to have a leg up in this area as they do take courses on gait analysis and biomechanics. Although I cannot be sure of the effectiveness of either physical therapists or trainers to see such problems. People have different areas of expertise, and until you see someone you know who can evaluate well it is basically a shot in the dark. Ideally, you will be able to find competent physical therapists or trainers in the area by word of mouth. That tends to be the best way of ensuring quality that I know of. However, I will do my best to educate you through this article.
Muscle and connective tissue evaluations
For most people muscular and connective tissue evaluations will be the easiest to do. This is because most of us know our bodies fairly well, and can tell when we have tight muscles, sore joints, or pain. Nonetheless, as we know from the previous few sections there are some things we can look out for to know some specific problem areas. In particular,
- Tight calves – look at plantar flexion and dorisflexion range of motion. Ideally, you should have a large range of motion in this area of at least 90-120 degrees of arc in the tibiotalar joint as defined by the angle made from the foot at the edge of its range of motion. If you can only obtain < 60-75 degrees of movement, you are at a more significant risk of injury.
- Weak glutes – There are various ways you can evaluate this. First, one way you can identify this is through light jogging. If you feel your quads working at all while jogging and running, you have very weak glutes. Similarly, if you cannot properly execute a squatting movement facing a wall with your toes 3 inches from the wall you probably have weak glutes. Likewise, if glute bridges make your quads and hamstrings burn from exertion, you also have weak glutes.
- Tight adductors – any sign of caving knees during movement is a universal sign for weak glutes and tight adductors. Also, this may be evaluated by attempting to go into a middle split. If you cannot obtain more than a 90 degree angle between your legs, you probably have very tight adductors.
- Plantar foot muscles and ankle stabilizers – if you cannot reliably single leg balance with shoes and barefoot for > 30s you are deficient in this area. You may not wave your arms around to help maintain balance.
- Quadriceps dominance and tightness – One of the ways to test the tightness of the quadriceps is to sit with your back against the wall on the ground. Then pull your leg towards you with your hands to the limit of its range of motion. After you let go with your hands, let your leg angle normalize which if you have tight quads it will probably start sliding away from you. Ideally, you should be able to get about 120-130 degrees of flexion or an angle of 50-60 degrees created with your knee. This is the minimum. For dominance activation testing, use the gluteal methods of analysis. Since glute strength and function is almost universally correlated with quadriceps dominance, you can use these tests to see how quad dominant you are. Remember, this is because as the hip extensors become more inactive, the load is shifted to the knee extensors.
- Tensor fasciae latae and IT band tightness – there are no reliable tests for this that I am aware of. However, you may be able to test to see how tight they are. Stand on one leg and keep a level pelvis, then try to adduct the other leg as far as possible past the other leg. If you cannot reliably get it more than a couple inches past the other leg, you are tight in the TFL and IT band especially if you feel them stretching.
- Hamstring tightness – Lie supine on your back with everything relaxed and straight legs. You should be able to bring one leg up to 90 degrees comfortably without bending either leg. If not, your hamstrings are indeed probably very tight.
- Deep butt muscle tightness – This stretch is a good test. If you cannot get your feet out more than a few inches away from the sides of your body then you are probably very tight. Work on improving the range of motion.
- Actual injuries – flat feet, plantar fasciitis, achilles problems, shin splints, non-other person ACL trauma, IT band syndrome, patellofemoral syndrome, SI joint pain, lumbar back pain, or any of the other joint deformities such as hallux valgus/bunions, talipes valgus, genu valgum/knock knees, etc. also signify problems.
As I started rereading through The Neanderthal No More series they wrote a lot of lower body dysfunctions as well. In part two, they included a lot of other tests you can do for the lower body to see if you have problems. Read through this as well and take notes.
Many of you will know by reading the above list and evaluating yourself that you have problems. Write them down and keep notes on what you need to work on. This is a good idea to add prehabilitation work focusing on improving these deficiencies which will improve muscle and connective tissue quality. This can be done in your warm ups or cool down times before and after your workouts respectively. For those that do not work out, you can do them whenever you have free time. This is encouraged for both the sedentary and athletes.
We will discuss in the next segment how to do soft tissue examination and optimization to correct many of these problems.
Alignment evaluations
The first posture deficiency that we will look at is how the hips, knees, and ankles/feet are orientated. When you are relaxed in the standing position, optimally they should all be pointed forward. The hips should not be externally rotated (so that the knees and feet point out). The knees should always point forward in line with the feet. The ankles should be oriented forward like the hips.
Now, in movements such as squatting it may be necessary to externally rotate the hips to safely descend in a squat. 0-30 degrees tends to be fine. The knees and feet should still be in alignment and the knees should track over the toes. However, in normal alignment this should not be the case. Loss of ability to attain normal standing posture translates to poorer ability to move well in activities like sprinting or jumping. If everything is not aligned correctly, force output is marginalized.
- Weight distribution — we naturally should have even weight distribution over each foot, and each foot will have even distribution of weight over the medially and lateral arches. The anatomical leg posture should be easily noticed and fixed by a physical therapist. If this is not an option, you may be able to do it yourself. If you have tight muscles or previous injuries you may note that you are still compensating by favoring one foot or side or different muscles. One of the ways to accurately see if you are favoring a certain side is to get two scales side by side and then stand relaxed on the scales. If you see a deficiency favoring one side you know you have a problem.
The medial-lateral weight distribution on the foot can most easily be tested through two different ways. The first way we want to test is seated on a flat surface with the feet hanging relaxed off the edge. If we have accurate weight distribution on the foot, we should be able to see that the ankle is neutral and the ankle/foot complex does not pronate or supinate while the muscles are relaxed.
The second way to test this is through single leg balance. If you are consistently favoring a side of the foot while balancing or tend to fall over one way especially you know you have weight distribution issues as well as balance issues. This can be fixed with practice balancing with proper shoes and barefoot.
Uneven weight distribution may be due to other factors such as injury or slipped SI joint, so everything is not set in stone. If you suspect that something in your body is off and cannot identify it then you should probably get yourself evaluated by a good physical therapist or chiropractor.
- Valgus alignment correction — for those of you who have flat feet/collapsing arches or plantar fasciitis, you know you tend to put more weight on the medial edge of the foot. In conjunction with restimulating the arch muscles and building up strength of the ankle stabilizers (which we will discuss in the next section), you need to start focusing on even weight distribution over the whole foot.
If you know specifically that the medial edge of the ankle tends to collapse down towards the floor and the tibia tilts inward then start your postural correction by holding the ankle in the inverted position. This will help lengthen the peroneals on the lateral side of the leg, and lengthen the inversion muscles on the medial side. Hold these positions for longer periods of time to help reset the muscle length just like static stretching.
Basically what we are doing is akin to postural realignment that you would do if you were trying to fix ‘caveman postural’ or shoulders forward. What you want to do is setup your posture into the correct position with shoulders back, head back, and chest out which will take a lot of energy at first until the body readapts to the correct posture. You will probably be sore if you are holding it at least 15-30 minutes a day, but once it improves you will notice a big difference.
- Varus alignment correction — one of the things we want to look for in the feet/ankles of supinators/varus stress is the muscles that are involved with inversion of the ankle are too short, the peroneals specifically for eversion are too long. When these muscles are out of balance, there is a strong tendency to roll and sprain the ankle. Ideally, the foot, when relaxed, should stay flat.
For example, when sitting down with the feet hanging off of the edge of a table you should be able to look down and see the foot oriented in the proper position. For supinators, the ankle will tend to invert by itself showing you more of the medial edge of the foot. This is the tendency for those that put more weight on the outside of the foot when walking or running and are likely candidates for inversion sprain. To focus on correction of this specific postural issue the peroneals on the outside of the foot need to be made stronger, and the neutral foot position must be held longer. No padding shoes and barefoot condition ensure that the foot may not invert during activity.
Shoes with padding tend to exacerbate the problem because the padding with which we put the most weight on sinks down further thus making us put more weight on the lateral edge of the foot in a cyclical pattern. This encourages repetitive ankle sprains. Thus, it is important to avoid any shoes with padding in the foot if you are one who sprains your ankles a lot.
What I have done specifically when I am in class or sitting at a desk is focusing on contracting the my peroneals and holding the foot in neutral or in eversion position for longer periods of time. This ensures that my muscles are getting used to a good alignment. In my case, it has taking a fair bit of constant work, but my foot posture is getting much better, and I have not had a sprain for a long time.
Note: It is very important that if your shoes have improper wear patterns such as uneven depression of the padding inside the shoe or lateral/medial wear patterns on the tread that you obtain a new pair of shoes. These improper patterns will continue to exacerbate injuries and teach you incorrect movement.
Movement analysis
First, it is important to analyze correct gait to ensure proper movement patterns. I would strongly suggest minimal footwear such as vibrams or no footwear at all when performing movement as it usually helps fix problems, and it will show problems as well.
- Squatting — squatting is a fundamental movement that everyone should be doing regardless of whether you are an athlete or not. We use it to sit down to chairs, get off our beds, use the toilet, and get up from the floor. Thus, it is a useful tool to evaluate problematic areas of movement such as (1) excessive pronation and weight stress over the medial arch, (2) inward caving knees, and (3) too much external rotation in the hips with compromised muscle flexibility.
If these three dysfunctions are present in training it usually means they have been there for a long time. Thus, it is important, especially for athletes, to have cues such as “spread the floor with your legs” to discourage the pronation and inward collapsing knees. And correctly setting up proper stance for squatting without an excessive externally rotated hip as this also encouraged collapsing knees with limited flexibility.
Proper squatting should emphasize initiation of the movement with the butt coming back first so as to ensure that quad dominance does not kick in especially with female athletes. The chest should be erect, and the lumbar curve intact. For beginners box squatting is preferential as it will allow the patient or client to emphasize more gluteal and hamstring strength as opposed to having the knees track too far over the toes which increases quad activation. Full depth is preferable in the squat to maximally engage the hamstrings. From there drive the chest up out of the whole and contract the glutes to close the hip ankle. You should not focus on pushing with the knees, but drive your force through your glutes, hamstrings and through your heels.

Dave Tate teaching box squats — Photo from http://thedriveforstrength.blogspot.com/
If the person or you have limited mobility such that you cannot maintain proper form in the lumbar curvature, you should go down as far as possible without compromising form.
Sometimes cues for spreading the floor are not enough. This is where the use of bands wrapped around both knees in squatting position can be effective. Basically, the person exercising has to force the knees out into the band to keep them tracking out over the toes to avoid valgus stress. This is important for activating the abductors and glutes especially. Stretching out the hamstrings and adductors between sets may also help significantly.
The first thing we would have you do is get back to the basics. Relearn how to third world squat. This will provide an excellent basis from which strengthening can occur. The series squat rx is probably one of the best to learn how to properly perform squats. I strongly suggest everyone watch this series whether you are a top level trainer or a complete newbie. Like wise, some books such as Starting Strength have > 40 pages dedicated to learning this movement properly. If you do not own this book, buy it and read it just for the squatting section.
I would strongly suggest that you lift barefoot if at all possible. Shoes with lots of padding especially make an instable base and limit not only the amount of weight you can lift but also do not train proper neural patterns because of the instability. There is a good case for unstable training, but it is better to be performed with bodyweight such as in balance work or on rings. With the heavier weights, barefoot is preferable if your gym does not kick you out and you are very careful about dropping weights on your feet.
Learning proper squatting technique from a qualified and competent trainer is optimal as they can see what you are doing wrong and provide the correct cues to correct improper movements.
The first step to correcting posture is knowing that you have an alignment problem, and then constantly remind yourself not to allow it.
Gait in walking and running
Gait itself in both walking and running is an issue. Unfortunately, gait is hard to analyze without a very keen eye and usually it will take a physical therapist who has been trained to do this. However, at higher intensities such as running and sprinting optimal technique tends to break down faster. Thus, it is important especially if you were a heel toe runner and/or have inward knee tracking or something out of alignment that you learn proper running technique.
The best way to ensure that you are running correctly is to do it barefoot in the grass. Start out with slow jogging. Incorrect foot contact and body movement is punished barefoot, and thus your body will usually naturally “revert” to correct technique. It would also be a good idea to video tape yourself to see if there are any movement patterns that your coaches or PTs can spot that are incorrect. If you pronate or supinate it is imperative that you be constantly aware of this problem during exercise. You need to be vigilant to correctly maintaining form even when barefoot running as well.
Interestingly, in one study running pattern is changed with barefoot vs. shoes conditions in experienced runners. Vibram fivefingers running pattern is most similar to barefoot. This may be a good option to learn correct running patterns if you do not like bare feet.
There are various systems on how to learn proper running technique such as CHI or POSE running. These are not necessarily needed but can be helpful if you are still struggling.
Gait (walking) is actually a very complex set of patterns which is why I am trying to simplify it like I did above. If you are interested in more information on how to correctly analyze something like this see this article.
Here are training tips and technique for barefoot running from a Harvard University blog.
Note: If you are new to moving around barefoot, keep the practice to a minimum at first: less than 200m. A lot of people are enthusiastic about strengthening their feet and do too much too soon which can also lead to a rash of overuse injuries. Start slow and build up volume as you can.
A bit on corrections
When correcting movement patterns as well as posture it is imperative that you be mindful. And what I mean by this is that you focus on it as often as possible. The easier you are able to hold correct posture and biomechanics, the easier it will be to get into the better groove for your body.
For instance, if you know that when you walk your knees tend to track in, it will often feel odd to have the correct form of knees tracking properly over the toes. Repeat the knees tracking over the toes often doing this mindfully. For posture it helps a lot to have stick notes in places where you are often such as on the computer reminding yourself to sit up straight, retract the scapulas, and hold the head back in proper position. The same is true with these lower body dysfunctions. Learn to hold your muscles in the proper position, and learn to move correctly by paying attention to everything you are doing.
As for desk placement if you have a desk job or are seated a lot. One of the recommendations that I have seen brought up in the comments which I totally agree with is getting a standing desk or a very low desk which forces a third world squat, or cross leg position on the ground. We would want to do this because both encourage better alignment patterns.
Both of the lower positions — cross leg on the ground and third world squat — encourage MUCH better mobility of the lower body which is lacking with people who regularly use chairs. Similarly, proper posture while standing avoids the excessive amount of time in hip flexion that causes a lot of the hip dysfunction prevalent in our society. Find out what works better for you and modify it.
I have discussed how to be aware of certain problems above. This is the first step. Now you have to take what you know and apply it. If you are a trainer or gym owner I would strongly suggest that you add mobility work as well as postural awareness and movement correction work to your warm ups and cool downs.
In the the next segment we will discuss soft tissue work that will significantly help with the corrections listed in this section. However, the fact that soft tissue work alone may correct injury conditions does not mean that it will correct they underlying dysfunctions. The importance of getting to the root of these problems should not be underestimated. You have to reeducate proper posture and movement patterns to your body by yourself.
Conclusion
In conclusion, we learned how to examine our bodies and movement patterns to identify problem areas with our muscles, posture, and movement.
Specifically with the muscles we looked at optimal flexibility as well as how to identify weakness and dominance in the muscles. In posture we learned to look for correct orientation of the limbs when standing naturally relaxed, and we also learned to look for even weight distribution to both feet and on both feet as well. For movement patterns, we looked at how to see problems with the fundamental movement of squatting, and how to be aware of problems involved in walking and running.
We already learned to be mindful, which is the most important part of correcting posture and movement patterns.
In the next segment we will discuss soft tissue optimization and correction. This is fundamental to maintaining proper health, staying pain free, and improving athletic performance.
6. Soft tissue optimization and corrections
In this part, I am going to discuss how to correctly find and optimize our soft tissue structures. This will improve our ability to stand correctly and move correctly. For those developing or who currently have injury conditions, this will provide a basis of how to correctly evaluate what you need to work on to help start you on the road to recovery.
I think that seeing a professional is always a good idea, especially if you had an acute injury. However, like I have said prior I cannot vouch for the quality of the professionals you see.
For those with injury conditions it is important to avoid aggravating exercises. With athletes the rehabilitative protocol should be the extent of your workout for those body parts especially if it is in bad condition. But that does not mean you can neglect other training that can be done – work on upper body, core strength, mobility, flexibility, or other sports specific drills. For those who are not injured but know they will be if they do not implement corrective exercises, add them to your warm up or cool down.
For non-athletes, I strongly suggest you start working out as well because of the benefits of exercise on health. However, you should not aggravate your condition. Working out improves blood flow and blood markers which will help you improve your conditions faster. Nutrition is extremely important in recovery so do not eat crap.
We will start from the feet and work our way up.
Feet and ankles
- Barefoot or minimalist shoes
First, it is important to go barefoot or minimalist shoes as much as possible. This will help ensure proper alignment of the talus and tibia as well as encouraging and rebuilding the ankle stabilizers and proprioceptors on the bottom of the foot.
Since shoes are a necessity for most of us as not having footwear is often times inappropriate. The type of shoes we want to aim for are with little to no padding as to allow a better feel of the ground. Remember the shoes for children study? Well, they do have recommendations about the types of shoes that should be worn. In light of the evidence we have investigated let us take a look:
- Quadrangular, to conform to the normal foot configuration, with abundant space for the toes.
- Flexible to allow free foot movement [especially at the ankle].
- Flat without elevation of the heel.
- Porous. Uppers should be made of leather or unsealed fabric to avoid skin maceration or fungal infections.
- Moderately tractive. Sole friction should be equivalent to that of the bare foot. Sole that are slippery (leather) or that create excessive friction (some rubber soles) should be avoided.
- Light weight to reduce energy expenditure.
- Extended above the ankle in the toddler to prevent shoe from slipping off during running.
- Acceptable in appearance because children are very sensitive about that.
- Reasonably priced. Medically satisfactory footwear need not be expensive.
I would clearly agree with all of the points except for the last two which need not be followed for proper foot health. Basically, what the study is describing is minimalist shoes. Since this article has come out, there are TONS of types of minimalist shoes now. Look for low to no padding in the shoe descriptions. Minimalist or “flats” typically have little to no padding.
If the feet are already deformed to the stress with conditions such as bunions, collapsed arches, or talipes valgus, then the alternative is orthotics if your condition is bad enough. These may provide relief, but you should still be doing rehabilitation as well. It is important to start correcting them right away.
- Balance work
It is important to progress to single leg balance work (standing on one foot) and eventually on unstable surfaces or with the eyes closed. Concentrate on firing the muscles in the bottom of the foot and the ankles to stabilize instead of waving your arms around to balance or moving the hips up and down. In fact, you should place your arms behind your back so you do not cheat. Aim to get 60s multiple times before trying to advance to harder progressions.
- Plantar muscle strengthening
For those who have collapsed arches, it is important to do foot flexor exercises to help stimulate the plantar aspect muscles to get stronger and take their role back to reform the arch. Putting a towel on the floor and scrunching it up with your toes, or picking up odd objects with your toes and putting them into a jar is a good way to do this. The same is true with plantar fasciitis.
My favorite thing to get the plantar muscles engaged is sand. If you have ever been to the beach and walked around for a while you may have noticed that all of the muscles in the feet get worked extensively and get sore. This is because sand is an unstable surface and is constantly changing. This will help get your plantar muscles firing again and hopefully get the arch back up to snuff. Start with low amounts of time (too much initially will make you very sore). Progressively work up to more as you get stronger.
Here is some information (thanks to Dan Pope for reminding me) about Janda’s short foot positioning that will help to increase proprioception as well as stimulate arch muscles:
- Soft tissue work
Roll your plantar fascia or use a golf ball to dig into it. Frozen water in a coke bottle may be very helpful for those with painful injury conditions on the bottom of the foot such as plantar fasciitis. If this is painful, you have something you need to work on.
Massage to the bottom of the foot, though awkward, is also a good tool to increase the mind-muscle proprioceptive connection. The way to do this is that you want the muscles in shortest range possible so they are not tight. Thus, you want to have your foot curled up itself, BUT not have the muscles contracted. Put the foot into plantar flexion and use one hand to curl your toes towards the plantar aspect of your foot and hold them. Use the other hand to massage. Focus on the sensations from the massage, and contract the plantar aspect muscles to stimulate activation.
- Foot drills
Foot drills are also good for proprioceptive awareness and help the body distinguish good movement patterns. Here is a web link.
If you are an athlete you should be doing these. No exceptions.
Notes
1. For those with the actual injury conditions such as plantar fasciitis, it is a good idea to go to a physical therapist.
2. As you may have figured out I do not like orthotics or “arch support.” At all. I believe they are, for the most part, a quick fix for problems that most people’s bodies have the capacity to handle given proper postural and biomechanical correction. Most of us were not born with congenital foot issues, and most of us do not have self-collapsing arches before adolescence. Of course, if you absolutely have to exercise such as military PT or you are competing in race season, they are fine. Similarly, those who may already have joint deformations may need orthotics to keep their conditions from worsening. However, I do recommend that you begin and start corrective exercises and tissue work to help start fixing the problem so you do not need them later.
3. One thing I have noticed in the physical therapy clinic I currently work at is that often those people with darker skin are more prone to pronation in the foot and collapsed arches. This may be due to Vitamin D deficiency. If levels of Vitamin D in the blood are low, proper bone growth and mineral density is decreased. Thus, this leads to bones that are softer and more likely to deform to the stresses we put on them. Couple this with the valgus stress of shoes and sitting, and you have an increased likelihood to develop flat feet, plantar fasciitis, and talipes valgus for those with darker skin. Since 80-90% of all people are Vitamin D deficient or severely deficient it would be a good idea to increase intake by getting out in the sun more, drinking more milk, or eating more fish. If, however, you cannot do these, then it is a good idea to supplement. In the link above there are some links to the cheapest (and highly rated) Vitamin D that I have found online at the bottom of the article.
4. Finally, like many of the conditions described just because you have patellofemoral syndrome does not mean you should be skipping these corrective protocols. In fact, it is important that you see if these exercise help your condition because in all likelihood they may as the lower body is a system and not compartmentalized. Keep this in mind as we continue.
The lower leg
- The calves
The calves are an obvious hot spot. As mentioned before Carson Boddicker’s Alleviating Ailing Ankles has videos of different stretches to do. Similarly, Kelly Starrett’s Your calves are tight bro is a good article to read on how to stretch them out. Find out what exercises work the best for you to improve your ankle mobility. Jacob Harden has some solid videos too.
As we have discussed before, the plantar fascia is continuous with the fascia of the rest of the posterior chain. People with plantar fasciitis especially usually have extremely tight calves. Loosing up the calves for people with foot problems often brings instant and continuous relief to such problems.
- Soft tissue work
It helps to get your calves with a foam roller or tennis ball. Golf balls are my preferred method of choice if you can tolerate it. It will hit all of the deep muscles under the gastrocnemius.
If you are going to do soft tissue work you want to have the muscle in a full contracted but relaxed position like described in the foot section. So have something hold your toe in plantar flexion, and bend your knee so that the gastrocnemius is shortened. For example, sit in front of the wall with the ankle up on the opposite knee, and use the wall to hold the foot in plantar flexion. Then use both hands to dig into your calves.
It is also a good use of time increasing plantar flexion through pointing the toes as well as loosen up the anterior tibialis as well. Especially if you are a now former heel-toe runner. Doing massage right before stretching is a good idea. Similarly, heat allows the muscles to loosen up and stretch farther than they would otherwise. Keep these two things in mind if you are having trouble loosening up the calves or any other muscle.
- Popliteus and plantaris muscles
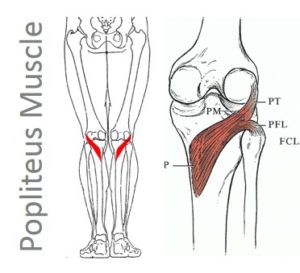
Photo from http://corewalking.com/
The popliteus muscle can get very tight in most people. To hit these use the same setup as above and target the area right below the back of the knee on the lateral side (so near the bottom of the leg that is up on the knee). Most people will have trigger points here even with no injuries.
The Leg
- Tight, strong quadriceps
Stretch them out and do tons of soft tissue work on them. Initially, foam rolling will probably hurt a lot, but as you get better progress to tennis balls and beyond. Additionally, do hip flexor stretches daily including before and after exercise. Find out which work the best for you.
For self massage target all of the muscles of the quad especially the rectus femoris as it will be very tight because it is a hip flexor. To put this muscle into shortest range of motion possible for massage, sit in a chair and prop up your leg so that it is straight and resting on a higher surface. From there you can dig into your quads with your fist. If you need more pressure and have the flexibility, lean over your leg and use your elbow.
- Tight, strong TFL and IT Band
Pretty much the same as the quads. Start with foam rolling, the work your way into tennis ball or golf ball. Additionally, do IT band stretches.
For massage you can target anywhere along the band that is tender as well as the TFL itself. For TFL massage sit in a chair with no sides and rotate the leg you want to work out to the side as far as possible while keeping your pelvis neutral. From there locate your iliac crest which is at the top of your pelvis at the midline of your body if you are looking at your body from the side. Follow it to the front until you encounter a sharp point. This is your anterior superior iliac spine (ASIS – also used for measuring Q-angle). The TFL is right below the space between the ASIS top of the iliac crest that we started at. Most people will be very tender here so dig in and loosen it up.
For the IT band use the same side hand of the leg that is abducted and grind your knuckles into the side of your leg. You can use the opposite hand to brace the leg to get more force. Most of you will find that the whole thing will be sore and tender.
- Tight hamstrings and adductors
These are two separate muscle groups, but I am grouping them together because there are several stretches that hit the both effectively. Firstly, I recommend proprioceptive neuromuscular facilitation (PNF) as the method of choice (for the quads and TFL as well if possible). Here is one way that hamstring and adductor stretches can be implemented. Gymnastics has a great set of straddle and ‘pancake’ or split exercises to help stretch out the hamstrings and groin as well. You can find some of them here.
Massage is going to be harder for both the adductors and hamstrings because it is difficult to hit the back and inner leg without lengthening the muscles. Ideally, you could have someone else do it, but that cannot always be the case. For the hamstrings, lie on your back and prop your leg up on a chair bent at the knee. From there loop your hands on either side of the affected leg and use your fingers to locate any sore or tender areas. You may also consider using a foam roller, tennis ball or golf ball is this is ineffective.
For the adductors you may hit them from the same position as the hamstrings. Alternatively, yo-nu can sit in the chair and use the same side arm to brace the leg. From there use the opposite arm to dig your knuckles into your affected leg. You can use your weight to drive the knuckles or your elbow into the tissue as you are massaging just like the quads.
If you are extremely quad dominant, you must focus on bringing up the hamstrings strength to bring back proper balance to the knee. This will most likely help with the knee disorders such as patellofemoral syndrome, IT band syndrome, and chondromalacia patellae.
Notes
Unfortunately, we cannot really do anything about ligament or meniscus issues. But if we ensure that the body is working correctly as a unit with correct movement patterns and muscle activation, then we do not need to worry too much about the connective tissue. Unless you are someone who works to the point of overuse injuries in which case you need to cut back and let your body heal.
Those with patellofemoral syndrome, IT band syndrome, and chondromalacia patellae will often have extremely tender quads, IT band and TFL. It is imperative to work out all of the kinks in the system, and stretch these muscles out to allow proper functioning of the knee. Similarly, tight adductors that need to be stretched will often contribute as will weak and tight hamstrings. Stretch out the adductors and hamstrings, and bring up the strength of the hamstrings.
For quad dominant athletes, you will also have extremely tight hamstrings and adductors. Loosen these up for optimal athletic ability. If you do not you should know that you are more susceptible to strains, and improper technique due to being too tight which may lead to more injuries.
The hips, SI joint, and low back
- The glutes
As I have indicated, the glutes play a major role in the dysfunction of the hip as their inactivation allows many bad things to happen to the lower extremities. This is because of their role in hip extension, abduction, and external rotation of the hip. The fact that they are inactivated leads towards lots of other muscle compensation which turns out bad for both the common person and the athlete.
Our first step is to get them activated again. Fortunately, Bret Contreras’ other article on the glutes is good for this. Do not skip phase I as easy as it may seem. This is needed to properly ensure and bring up activation in the glutes, especially if you have a desk job. Both parts of phase I must be followed because the first helps to activate your gluteus maximus and the second helps to activate the gluteus medius. Activating both of these are important for lower body health as we discussed earlier.
From there follow phase II, III and IV to bring up hypertrophy, strength, and power. This is important especially if you are an athlete as it will make you more explosive. If you are not an athlete, this will be important for you anyway to correcting your own posture and biomechanical dysfunctions we mentioned earlier.
Alternatively, Kelly Baggett’s No glutes = no results is also very good at illuminating this problem. His article includes some postural evaluations as well as a basic program which may help. You should read both. Here is a good exercise from Nick Tumminello called the super bird dog which will show you if you are making progress with glute activation. Ideally, it should be easy.
If you have a desk job it is a good idea to get up every 20-30 minutes and do some glute exercises or at least squeeze your glutes so that you can increase activation and develop a good mind-muscle connection. If you have the possibility to stand a lot, that may be an option as well. Basically, our goal here is to minimize the problems associated with constantly sitting all of the time. By doing activation work and/or strengthening for the glutes very often we build a much stronger neural connection to them which will improve their activation in compound movements such as walking, stairs, running, squatting, and weightlifting activities.
If you can bring a foam roller or other device to help stretch out the hip flexors all the better. Here is a good video on utilizing a foam roller for the hips that can be used to help loosen up the area.
Finally, traumatic ankle injuries, (2) & (3), such as sprains have detrimental effects on the hip extensors like the glutes which lead to quad dominant compensation. Obviously, this is not good for athletic performance or normal life. So it is important if you have sprained a lower extremity to systemically rehabilitate yourself rather than just focusing at the ankle.
- Tight intrinsic butt muscles
Hitting and loosing these up is actually very easy and feels very good (no puns intended). This is the stretch I prefer as opposed to the piriformis stretch lying on the back with the leg crossed over and pulling. This one encourages a better lumbar position and is a bit more friendly on the knee by keeping it from torquing.
The other way you can loosen them up is with the internal hip rotation stretch such as this. Another soft tissue technique to loosen up the muscles is to use a tennis ball and basically sit on it. This can be done sitting down onto it if you need more pressure, but the muscle will be shorter when you lie down and move your glutes around on it. Try both and see which one works better for you.
It is important after you loosen these muscles up to do some strength work, to ensure they won’t simply tighten back up. Here are some basic exercises:
- SI joint and lumbar stability
Obviously, with these joints you want decreased mobility and more stability as we discussed before. So it is imperative to increase core strength.
I am going to only discuss basics here, but I do prefer that development of the full body lifts are critical for developing a strong core. If you are specifically injured and an athlete, the core lifts such as squats, deadlifts, etc. may be contraindicated with some specific lower body dysfunctions. If any exercise is emphasizing improper biomechanical movement or pain, it is best to avoid it for now.
Supine posterior pelvis tilts, planks with the pelvis posterior tilted, bird dogs, upright bird dogs, supermans, etc. are all basic core exercises to get you started.
Notes
By now you should have a greater understanding of lower body anatomy and potential solutions for your dysfunctions. Usually tender or tight areas will tend to mean that something is out of balance or you have let your tissue quality become poor. Your health and performance will only improve by fixing these troubled areas.
It is in your best interests with any of the injury conditions I mentioned (and even possibly some I did not mention) to evaluate your body and find all of the different trigger points or tender areas and eliminate them. Foot conditions such as bunions and flat feet can be affected by inactivated glutes especially gluteus medius, while lower back pain can be caused by problems down in the foot. This is in addition to the rehabilitative protocol specific to your condition that I mentioned.
Use the list that you wrote down in the last section and go through the specific soft tissue work I have listed and start working out the kinks.
As I have been harping on the Neanderthal Series great. Here is their take on rehabilitative protocol and reintroduction of lifting exercises. This is whole body so you may have to pick out the core/lower body work out from the upper body. I would suggest this as a read through if you want a non-focused program you can follow; however, you should definitely still target specific tight tissues with above soft tissue work as well. Here’s a shorter version focused solely on the hips from Mike Robertson.
Certain injury conditions
Now that we have discussed most of the specific work I am going to talk specifically about some of the injury conditions. It is an extremely good idea to hit up all the different muscles and other exercises I mentioned to see if you are tight, tender, or need strengthening in those areas.
Rather than me specifically telling you what to do you will be able to figure it out for yourself. I will go over some of the main points of each of the injury conditions that I have mentioned as some guidelines. This is by no means complete. If you wish to have professional advice and a plan optimized towards your health, see a physical therapist.
As we discussed, there are multiple things you should be checking with any of the injury conditions. These include the (1) inward tracking knees during normal standing posture, movement, or exercise, (2) reactivation and strengthening of the gluteus maximum and medius, (3) increase calves mobility especially if your dorsiflexion ROM is bad (bent leg stretching for soleus, straight leg for gastrocnemius), and (4) loosening up the adductors. These should be done in all of the injury cases I am describing below.
- Flat feet / pes planus / collapsing or collapsed arches – focus needs to be stimulating and strengthening the plantar aspect muscles and improving balance. It really depends on how long the arch has collapsed if it can fully reform before the bones have totally deformed to the collapsed orientation. Improving glute function and calf mobility is a must. If the condition has lasted for long periods of time, orthotics may be indicated especially with varying degrees of pain as well as preventing the arch from further collapsing. Again, ideally we want to not have to use orthotics, but sometimes they are necessary.
- Hallux valgus – Treatment may vary depending on the orientation of the joints. Generally, restoring proper biomechanics and weight distribution will help the most, as will the same foot exercises described the flat feet section. Improving glute function and calf mobility is a must as is correcting weight distribution patterns. Improper footwear can also be a cause so be wary of that.
- Plantar fasciitis – Same as flat feet, especially if you have flat feet and this condition. For plantar fasciitis in particular, night splints can be effective.
- Achilles tendonitis – First, read this on tendonitis. Second, fix your running form and/or avoid high impact scenarios to let it heal. If you have a valgus condition in particular this will exacerbate it so be sure to focus on correcting this improper movement pattern.
- Sprained ankles – Depends on the severity of the sprain. Surgery may be needed or not. First, focus needs to be on reducing the swelling, and restoring range of motion with painful stretching. Secondly, strengthening and balance must be improved. Also, as noted by the studies focus on proper gluteal strengthening as well. Be sure not to compensate a lot on the opposite leg. This will cause muscular imbalances that are very difficult to get rid of.
- Shin splints – Focus on fixing proper movement patterns especially running. The improper heel-toe running is one of things that exacerbates this condition the most. Strengthening the anterior tibialis and loosening up the calves will help significantly.
- Patellar tendonitis – Same as the achilles. First, read this on tendonitis. Second, fix your running form and/or avoid high impact scenarios to let it heal. It is very important to stretch the quads, TFL and IT bands thoroughly, and improve glute and hamstring strength as well as ankle mobility.
- Patellofemoral syndrome / chondromalacia patellae – Focus needs to be on the entire upper leg-hip complex by restoration of correct tissue function and movement patterns. For those of you who missed the boat that is the calves, quads, hamstrings, TFL, IT band, glutes (both), and butt muscles.
- IT band syndrome – Focus needs to be on the entire upper leg-hip complex by restoration of correct tissue function and movement patterns. For those of you who missed the boat that is the calves, quads, hamstrings, TFL, IT band, glutes (both), and butt muscles.
- Ligament or meniscal damage – See an orthopedic doctor. If you are past a surgery such as ACL repair, this study may interest you. Focus on restoring proper movement patterns, and regaining proper strength ratios in the leg. Gluteal strengthening will help out a lot to reduce the amount of force at the knees.
- Joint deformities – Depending on severity orthotics or other things may be indicated. Even so, proper movement patterns should alleviate problems, but it is going to be a long uphill battle. See the appropriate medical professional.
Conclusion
Extensive use of manual soft tissue work is the key to rehabilitating injuries. Just like I listed the importance of massage in On Tendonitis, I fully expect if you are trying to recover from a lower body injury or are close to one that you do an extensive analysis of your soft tissue quality and movement patterns as I described above. This information should set you on the road to recovery and help you maintain optimal athletic ability or get back to your daily life pain free. In conjunction, for those who do not exercise, it will significant improve your quality of health.
This concludes this section. In the next, I will give a summary and the key points you should be taking away from this article. Also, I will provide a large list of links that may provide additional help to those of you suffering with injuries or other information on the topics I have discussed.
7. Final Conclusion
We have extensively looked at the valgus conditions that are prevalent in modern society. These are because shoes and sitting lead to mechanical deficiency that allows problems to develop. Let’s review.
Shoes tends to cause the problems of
- Tight calves resulting in loss of 10-20 degrees of dorsi-flexion ROM in the calves.
- Inactivation of the muscles on the bottom of the foot and the ankle stabilizers
- Decreased proprioception of the lower limb
Sitting tends to cause the problems of
- Inactivation of the gluteal muscles.
- Tight hip flexors (iliopsoas, rectus femoris, sartorius, tensor fasciae latae (TFL), and adductors longus and brevis).
These problems tend to lead to inward tracking knees.
Inward tracking knees tends to cause the problems of:
- flat feet / collapsed arches / pes planus
- plantar fasciitis
- achilles tendonitis or rupture
- patellar tendonitis
- ACL sprain or rupture
- quadiceps dominance and tightness
- TFL and IT band tightness
- hamstring weakness and tightness
- joint deformities like bunions, collapsed arches, talipes valgus, knock knees, etc.
Remember, many people may have multiple symptoms described above, but usually they only manifest one injury. Only one or two parts may tend to “break” and cause a person pain before they can do enough damage to incapacitate other parts in the chain. It is important that everyone evaluate their lower body posture and movement patterns to ensure that such things do not occur.
- Barefoot and/or minimalist shoes
If you are starting to go barefoot after wearing shoes all your life be wary. Initially, there will be decreased ability to maintain balance. This is because our bodies have “adapted” to shoe use. However, once adaptation back to barefoot or near-barefoot conditions occurs, balance and gait should be significantly improved.
Learn to run and move correctly with minimalist shoes or barefoot. We previously talked about barefoot running in grass being a good alternative to start with. Any type of shoes with extremely thin soles are good as well, but they must have low cut sides that allow proper ankle mobility. Integrate this training with the foot drills and balance training.
Start VERY slow. Since most people’s feet are not adapted to moving around barefoot a lot doing anymore than even 200m in grass is questionable. When you are first starting to exercise you would not do 200 repetitions of pushups, so why would you do as many repetitions running?
Weightlifting shoes are fine for weightlifting since ankle mobility needs to be good to lift well anyway.
As for the minimalist shoes we discussed this in the last segment. This is what we are looking for:
- Quadrangular, to conform to the normal foot configuration, with abundant space for the times.
- Flexible to allow free foot movement [especially at the ankle].
- Flat without elevation of the heel.
- Porous. Uppers should be made of leather or unsealed fabric to avoid skin maceration or fungal infections.
- Moderately tractive. Sole friction should be equivalent to that of the bare foot. Sole that are slippery (leather) or that create excessive friction (some rubber soles) should be avoided.
- Light weight to reduce energy expenditure.
- Extended above the ankle in the toddler to prevent shoe from slipping off during running.
- Acceptable in appearance because children are very sensitive about that.
- Reasonably priced. Medically satisfactory footwear need not be expensive.
I would clearly agree with all of the points except for the last two which need not be followed for proper foot health. Basically, what the study is describing is minimalist shoes. Since this article has come out, there are TONS of types of minimalist shoes now. Look for low to no padding in the shoe descriptions. Minimalist or “flats” typically have little to no padding.
- Negating Sitting
Standing desks workstations are becoming more popular for those with desk jobs, and they’re pretty cheap now compared to how much they cost even a few years back.
It is important to be doing a lot of gluteal activation work as well as stretching out our hip flexors. Everyday if possible. Get particular activation exercises into your warmups and cooldowns. Add specific strengthening in your workouts. Include soft tissue work for the tight muscles.
If you are someone who does not exercise then you should exercise! Exercise is not only healthy but a good stress reliever. However, if you still refuse, it is still a good idea to do these exercises sometime in your day whenever you choose.
Now, for those of you looking to get ahead of the game: yes, you can do them at any time. It may be a good idea every 20-30 minutes if you have a desk job to stretch out the hip flexors and do some glute activation work. Just do not let anyone catch you doing glute bridges or other hip thrusting exercises on the floor otherwise it may be awkward. Stretching can probably be explained away though. 🙂
- In workouts
Hopefully most of us have competent trainers who knows correct movement patterns as well as the cues to correct them. However for a lot of people this is not the case.
For the people who do not have anyone to correct their technique during exercise it is a very good idea to invest in a video camera and find a good online fitness community who is willing to take a look at others’ exercises and help them correct any flaws.
Investing in books or reading material online about correct technique for exercises is imperative for anyone who exercises. Books such as Starting Strength have extensive chapters on technique alone to make everything as safe and effective as possible. The best way to improve very quickly is perfect technique because it allows you to lift the most weight or perform at the highest intensity effectively.
- With developing or current injury conditions
Get to know your body! If you do notice that certain movement patterns are askew, then it is a good idea to get yourself evaluated by a good trainer or get evaluated by a good physical therapist who knows a lot about exercise.
If you have developed a condition, it is not an all or nothing proposition. You do not have to completely stop working out – you can keep doing skill work, upper body, or core work if you have a lower body injury. But you definitely should not be pushing through the pain with a “no pain no gain” attitude.
One last thing that is a very important reminder that I have stated earlier as well. One thing I have noticed in the physical therapy clinic I currently work at is that often those people with darker skin are more prone to pronation in the foot and collapsed arches. This is due to Vitamin D deficiency. If levels of Vitamin D in the blood are low, proper bone growth and mineral density is decreased. Thus, this leads to bones that are softer and more likely to deform to the stresses we put on them. Couple this with the valgus stress of shoes and sitting, and you have an increased likelihood to develop flat feet, plantar fasciitis, and talipes valgus.
- Final Words — basically if there was a few key points to take home then know these.
Shoes and sitting tend to lead to the loss of ankle and hip strength, proprioception, and mobility translates to increased stress at the foot arches, knees, and SI joint/lower back. This leads to lower body dysfunctions.
Essentially, your arch, knee, and lower back problems can be solved by (1) focusing on stability and proprioceptive work at the painful joints in question, and (2) improving your strength and mobility in the hips and ankles. Point 2 is one of the most critical points that is often overlooked by most coaches as well as physical therapists. Remember, I have referenced studies and logically walked you through the physiology that shows arch, knee, and lower back pain can be cured or will show significant improvement through increasing flexibility/mobility and strength in the ankles and hips.
Thus, shoes and sitting are universally detrimental to the development of chronic lower body conditions. Counteracting these stimuli should be focused on restoring proper ankle and hip function, and focusing on stability at the arches, knees, and SI joint/lower back.
- Do mobility work, soft tissue massage, and strengthen/stretch the appropriate musculature.
- Be mindful about posture and your movement patterns.
These two steps are the key to your improvement and overall health. Prehabilitation work is always better than getting an injury have having to take time off out of your schedule to do rehabilitation. If you are rehabilitating, then do everything you can in your power to get back to good health. No one likes to be injured.
Hopefully, this series taught you how to prevent and rehabilitate lower body dysfunctions.
References
Most of the references I linked in the above sections. Here are some other articles for you that discuss some of the physiology and corrective nature of the work I am talking about above.
- Trigger points, More trigger points
- flat feet, Flat feet
- Sacroiliac mobilization I, Sacroiliac mobilization II
- The low back
- lower back savers I, lower back savers II
- Pain free lower body posture
- ACL Injuries & Young Female Athletes
- Preventing Hamstring Injuries
- The Female Knee, the Athletic Knee
- Solving Anterior Knee Pain
- Healing the Hips
- Teach them to land first
Thanks for reading. Feel free to comment. If you enjoyed this article or think it would be useful to people you know, send it your friends.
Disclaimer: Any information contained herein is not professional medical or physical therapy advice. Always consult your doctor or physical therapist before using such information. For more details see our full site terms and conditions.
This article was originally published November 22nd, 2009 on Eat Move Improve. Updated Dec 2016.
Questions about articles may be addressed to the Overcoming Gravity reddit.
Author: Steven Low
Steven Low is the author of Overcoming Gravity: A Systematic Approach to Gymnastics and Bodyweight Strength (Second Edition), Overcoming Poor Posture, Overcoming Tendonitis, and Overcoming Gravity Advanced Programming. He is a former gymnast who has performed with and coached the exhibitional gymnastics troupe, Gymkana. Steven has a Bachelor of Science in Biochemistry from the University of Maryland College Park, and his Doctorate of Physical Therapy from the University of Maryland Baltimore. Steven is a Senior trainer for Dragon Door’s Progressive Calisthenics Certification (PCC). He has also spent thousands of hours independently researching the scientific foundations of health, fitness and nutrition and is able to provide many insights into practical care for injuries. His training is varied and intense with a focus on gymnastics, parkour, rock climbing, and sprinting. Digital copies of the books are available in the store.

